In this article:
Pregnancy is undoubtedly the happiest period in a woman’s life, but even it can sometimes be overshadowed by all sorts of troubles and pathologies. One of these pathological conditions during pregnancy is polyhydramnios, which must be treated.
The composition of amniotic fluid changes throughout pregnancy, so it is important to monitor its amount at each trimester.
Polyhydramnios is the appearance of an excess amount of amniotic fluid, significantly exceeding the norm. The diagnosis of polyhydramnios can be made to a woman at very different stages of pregnancy. Such complications occur in 1 in 100 pregnancies.
During the normal course of pregnancy, the necessary amount of amniotic fluid is formed for the development of the fetus, approximately 1000-1500 ml. Amniotic fluid consists of 97% water, which contains proteins, calcium, chlorine and sodium salts. Thus, the baby receives oxygen, necessary nutrients and reliable protection from the external environment. Also, the embryo can calmly move and swim in the mother’s stomach, and make movements with its limbs.
Amniotic fluid is the environment in which the fetus develops. The water temperature is 37 degrees.
Properties of amniotic fluid:
- Amniotic fluid protects the embryo from shocks and shocks. In addition, noise coming from the outside world is also muffled.
- Amniotic fluid protects the umbilical cord from compression between the uterine wall and the fetus.
- Amniotic fluid helps reduce pain during contractions.
- They help open the cervix during childbirth.
- The bladder, which contains the fetus and amniotic fluid, creates an airtight shell into which nothing can enter from the outside.
- Amniotic fluid contains immunoglobulins.
The amount of amniotic fluid changes every week. Therefore, each trimester of pregnancy has its own norms. At the very beginning of pregnancy, the amount of amniotic fluid is approximately 30 ml. At 23 weeks, the amount of amniotic fluid is about 600-700 ml. By 30, 32, 33 and 34 weeks this figure is approximately 600-900 ml. By the 36th week, the amount of water increases to 1000. At the 37th and 38th week of pregnancy, the amount of amniotic fluid becomes maximum. At 39 weeks and closer to the birth itself, a decrease in amniotic fluid to 800 ml is observed.
In the presence of certain predisposing factors, the amount of water may decrease or increase. When amniotic fluid is less than normal, this condition is called oligohydramnios. Oligohydramnios is also a pathology and affects the development of the fetus and the condition of the pregnant woman.
Causes of polyhydramnios
Although the causes of polyhydramnios have not yet been fully studied, there are some factors that contribute to the occurrence of this pathology.
Polyhydramnios during pregnancy can occur due to the following reasons:
- pathology of fetal development;
- infectious diseases of a pregnant woman;
- bacterial infection;
- diseases of the cardiovascular system;
- Rh conflict between mother and fetus;
- metabolic disease;
- diabetes;
- pyelonephritis;
- multiple births;
- large fruit.
Types of polyhydramnios
This condition in a pregnant woman can occur in different ways: acute or chronic. There may be severe or moderate polyhydramnios.
The acute form is characterized by a violation of the general condition of the pregnant woman and the fetus. Such births, as a rule, end in miscarriage, stillbirth, or such a child will have developmental defects. Polyhydramnios occurs in acute form, usually from the 16th to the 24th week. Sometimes the amount of amniotic fluid may increase even within a few hours. In this case, immediate medical attention is required due to the dangerous condition.
Moderate polyhydramnios during pregnancy is characterized by a gradual increase in symptoms and signs. Moderate polyhydramnios can lead to the birth of a child with developmental abnormalities. This is due to a constant lack of oxygen. Very often, moderate polyhydramnios occurs in a chronic asymptomatic form, and therefore can go unnoticed for a long time.
Signs of polyhydramnios
Sometimes a pregnant woman herself may suspect that she has polyhydramnios, based on the presence of some signs characteristic of this condition.
- The abdomen of a pregnant woman with an excess amount of amniotic fluid reaches a circumference of more than 100 cm. It has a slightly rounded shape. There is a feeling of heaviness in the stomach and back. The uterus increases in size and begins to compress internal neighboring organs. Therefore, as a result, a pregnant woman often experiences shortness of breath and other ailments.
- The lower extremities may swell. In some cases, early rupture of amniotic fluid may even occur.
- A fluctuation appears: the pregnant woman can quite clearly hear gurgling in her stomach. There is pain in the perineum.
- A large number of stretch marks appear on the stomach.
- A pregnant woman's pulse quickens. The fetal heartbeat is faintly audible.
- Since more free space appears, the fetus takes an incorrect position in the uterus (pelvic, oblique). This is directly reflected in the birth itself: the distended uterus contracts incorrectly and labor with polyhydramnios will be characterized by weak labor.
Polyhydramnios is also dangerous because the child can become entangled in the umbilical cord. Hypoxia may develop and the fetus will not receive enough oxygen. Even if the birth takes place on time, the fetus may have intrauterine pathology; such a child may be born with a violation of the development of internal organs or systems.

It should be remembered that the earlier polyhydramnios appears in a woman, the more amniotic fluid accumulates and the risk of complications increases.
Moderate polyhydramnios
The diagnosis of moderate polyhydramnios is made when the amount of amniotic fluid is approximately 1.5 or 2 liters. And although such a diagnosis is made even in the first trimester of pregnancy, one can seriously talk about the presence of pathology only after the 16th week. The cause of this condition is often a Rh conflict between mother and fetus or the presence of infections.
A woman with moderate polyhydramnios feels tension in her abdomen. It becomes more elastic. When you palpate the fetus, you will notice that it often changes its position. You can hear water rolling in your stomach. The uterus increases in size and becomes swollen.
Moderate polyhydramnios can be determined through a routine ultrasound examination or examination. Moderate polyhydramnios is characterized by early labor and placental abruption.
A pregnant woman with moderate polyhydramnios should be constantly under the supervision of specialists, since sometimes it happens that this diagnosis is erroneous or temporary.
In the absence of serious pathology, the doctor tries to maintain the pregnancy and ensure that the birth takes place naturally without artificial intervention. Conservative treatment is prescribed: vitamins, hypothiazide. If necessary, antibiotic therapy is administered.
Polyhydramnios at the end of pregnancy
Polyhydramnios at the end of pregnancy accounts for approximately 0.6% of all other pathologies. Its appearance may be caused by late toxicosis. This can lead to serious complications during childbirth:
- umbilical cord prolapse;
- oxygen starvation of the fetus;
- weakness of labor.
Therefore, such a diagnosis is an indicator for carrying out. Treatment for such polyhydramnios depends on the cause.
Diagnosis of polyhydramnios
Polyhydramnios can be diagnosed by examination by a gynecologist at an appointment at the antenatal clinic. To do this, the doctor examines the pregnant woman for the presence of relevant signs. The most reliable method for diagnosing polyhydramnios is ultrasound examination. Doppler ultrasound is also prescribed. Thus, it is possible to detect a more accurate amount of amniotic fluid and check the blood flow in the umbilical cord and placenta.
A thorough examination of the fetus allows you to identify possible abnormalities in its development.
Polyhydramnios can be diagnosed using the “amniotic index”. There is a special table that allows you to determine the normal amount of amniotic fluid in a certain trimester of pregnancy.

If the diagnosis is confirmed, the woman is sent for additional examination of the fetus.
Consequences
With polyhydramnios, the following consequences are possible:
- or termination of pregnancy;
- fetal death or developmental defects;
- if the cause of polyhydramnios is an infection, then there is a possibility of infection of the fetus;
- prolapse of the umbilical cord or fetal arm (leg) during childbirth;
- the presenting part of the fetus does not descend during labor or is not fixed;
- malposition.
- bleeding;
- various gestoses.
Treatment
The main treatment for the diagnosis of polyhydramnios is aimed at eliminating the cause that caused this pathology. First, the expectant mother undergoes all the necessary tests confirming the presence of polyhydramnios: fetal cardiotocography, ultrasound examination, blood test for Rh factor, Doppler sonography and others.
As a rule, complex treatment is carried out. In case of moderate or unexpressed pathology, the pregnant woman is prescribed drug therapy. Depending on the woman’s condition, treatment can take place in a hospital setting or at home (outpatient). This condition does not require termination of pregnancy or delivery.
Diuretics (diuretics), vitamins and antibiotics are prescribed. Antibiotics are necessary to fight microorganisms, since the main cause of polyhydramnios often lies in the infectious process. Also, from 24 weeks to 38 weeks, indomethacin is prescribed.
If the prescribed treatment does not help or the polyhydramnios becomes severe, then the doctor prescribes early delivery. Medicines are used to artificially induce labor.
During artificial delivery, it is necessary to carefully open the membranes and gradually release amniotic fluid so as not to cause fetal asphyxia. This procedure is carried out using a thin catheter. Measures are taken to prevent the prolapse of the umbilical cord or fetal limbs.
Medicines to stimulate labor should be used no earlier than 2 hours after the amniotic fluid is released.
In the early stages, when delivery is impossible, amniotic fluid is released. Amniotic fluid helps the baby move through the birth canal, regardless of artificial or natural opening of the membranes. But this should be done carefully so that the umbilical cord does not fall out.
If the fetus has developmental defects that are incompatible with life, then the pregnancy is terminated at up to 28 weeks.
Childbirth
If polyhydramnios does not affect the condition of the pregnant woman or her fetus, then childbirth is carried out naturally. A mandatory procedure in this case: artificial opening of the amniotic sac. In this case, the volume of the uterus decreases, and this helps make contractions more productive. Often such labor is delayed, and then there is a need for labor stimulation. Labor stimulation is carried out by introducing labor accelerating drugs. And as a last resort, a caesarean section is performed.
The postpartum period may be complicated by bleeding due to poor uterine contractility. Therefore, the woman is prescribed the introduction of contractile drugs such as oxytocin and methylergometrine.
Prevention of polyhydramnios
Since polyhydramnios is a pathology, this condition can be avoided if precautions are taken.
It is very important to immediately rule out the presence of Rh conflict. During pregnancy, a woman should move as much as possible. It is necessary to calculate the amount of fluid taken. It also wouldn't hurt to adjust your diet a little.
To prevent polyhydramnios, the expectant mother should take vitamin complexes or medications prescribed by a doctor.
It is necessary to undergo all examinations and tests on time, as they will help to identify pathology or deviations in fetal development at the earliest stages.
In this case, you can avoid serious consequences during childbirth and the postpartum period. It is important to remember that regular examinations by an obstetrician-gynecologist are not just a formality, but a vital necessity on which the baby’s condition depends.
Useful video
Around the baby in the womb there is amniotic fluid, which is vital for its safety and development. These waters protect the fetus from mechanical shocks, infections, temperature changes; they are important for the formation of breathing and digestion processes, as well as for the development of the baby’s bones and muscles. What is polyhydramnios? This is when too much amniotic fluid accumulates in the uterus; this diagnosis occurs in 1% of all pregnancies.
Types of polyhydramnios
Relative - not dangerous if the doctor is absolutely sure that the pregnant woman does not have any infection. It is most common in women who are expecting a large child.
Idiopathic - polyhydramnios, the cause of which remains unclear.
Moderate - the size of the vertical pocket is 8-18 cm.
Pronounced - the size of the vertical pocket is above 18 cm, and more than 24 cm.
Borderline, tendency to polyhydramnios - when the level is at the borderline between normal and elevated levels. Observation required.
Acute - when the amount of water increases at a high speed. Quite dangerous for the life of the fetus if no measures are taken by doctors.
Chronic - the amount of fluid is higher than normal, but stable.
Causes of polyhydramnios during pregnancy
 Experts say that it is possible to find out the causes of polyhydramnios only in 2 out of 3 cases. It turns out that one third of pregnant women with this diagnosis have idiopathic polyhydramnios (for no apparent reason). Why might a woman have this problem?
Experts say that it is possible to find out the causes of polyhydramnios only in 2 out of 3 cases. It turns out that one third of pregnant women with this diagnosis have idiopathic polyhydramnios (for no apparent reason). Why might a woman have this problem?
- Uncontrolled diabetes mellitus in a woman.
- Multiple pregnancy. In most cases, it happens that one child receives more blood and nutrients than the other, which leads to complications.
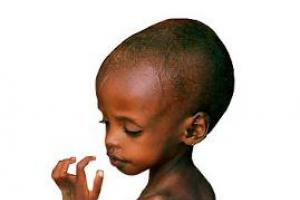
- Anomalies of fetal development. In this case, it may be difficult for the child to swallow and process the amniotic fluid. This occurs due to a cleft lip or palate, hydrocephalus, problems with the gastrointestinal tract, nervous system or heart.
- Fetal anemia.
- Cardiovascular diseases in pregnant women.
- Incompatibility of blood between mother and child.
- Problems in the functioning of the placenta.
Signs and diagnosis
If we are talking about a mild form, then usually the woman does not feel any suspicious abnormalities.
If the case is severe, shortness of breath, swelling in the lower abdomen and rare trips to the toilet occur.
Polyhydramnios is usually diagnosed after an ultrasound. It may be prescribed unscheduled if the gynecologist suddenly notices some signs - high blood pressure, a urinary tract infection suddenly appears, the stomach becomes larger than normal and swelling appears.
Treatment methods
If polyhydramnios is acute, an amniotomy will be prescribed to remove excess water. If it is chronic, it would be better to prolong the pregnancy until the due date and prescribe complex therapy.
Is it possible to cure yourself at home using folk remedies? I strongly recommend that you follow your doctor's instructions and not use any herbal remedies or homeopathy. There are a number of drugs that are used depending on the cause of polyhydramnios, we will discuss them in detail below. Leave folk remedies for treating colds.
What does an obstetrician-gynecologist usually prescribe?
- Actovegin, Curantil. These drugs are prescribed to everyone, at the slightest deviation from the norm. Whether or not to use them for prevention is the decision of every woman. Here are interesting data on each of the drugs: Curantil and Actovegin.
- Antibacterial drugs (Amoxiclav, Ampicillin, Vilprafen, Rovamycin, Cefazolin). Some of them are prohibited during pregnancy, but their use is possible if the benefit outweighs the possible risk. In most cases, with polyhydramnios, the infection that led to it is detected. Tests should be taken to determine which antibiotic these bacteria are hypersensitive to. This method is much more effective than simply drinking a randomly selected drug for prevention.
- Wobenzym. Preparation of animal and plant origin. Used in complex therapy with antibacterial drugs.
- Diuretics (Canephron, Hypothiazide).
- Indomethacin. Decongestant and anti-inflammatory drug. Helps normalize fluid levels.
- Vitamins.
Expectant mothers can face the problem of increasing the amount of amniotic fluid at any time, but the biggest concern among doctors is polyhydramnios during late pregnancy. Do you know why?
It turns out that at this time, pathology can provoke, at best, premature birth, and at worst, bleeding during labor, or even completely jeopardize the health and life of the baby. And you can prevent it and identify it yourself, the main thing is to know how.
The baby is surrounded by amniotic fluid in the womb. It performs several functions at once: it protects, provides freedom of movement, takes part in metabolic processes, and is also responsible for the development of basic skills in the fetus (swallowing, motor skills). They say that it smells like milk, and this explains how a newborn baby finds the breast so quickly.
Nature intended that this liquid be regularly renewed. That is why its volume is different at different periods:
- at 10 weeks – this is about 10 ml;
- at 14 – 100 ml;
- at 21 – 22 – 400 ml;
- at 30 – 32 – 700 ml;
- at 37 – 38 – up to 1500 ml (this is the maximum);
- at 39 – 40 – about 800 ml.
This is ideal. And if the volume significantly exceeds the norm, polyhydramnios is diagnosed. As a rule, doctors are alarmed by a significant excess - 1.5 - 2 times. The most interesting thing is that modern medicine distinguishes between several types of polyhydramnios, sometimes making a borderline diagnosis that sounds like a “tendency to polyhydramnios.” In other words, there is no pathology yet, but the risk of its development has been identified.
How to suspect and identify
To answer this question, it should be recalled that there are two stages of polyhydramnios: acute and chronic. Moreover, the signs in both cases are the same, the difference is only in the speed of their manifestation.
In the first case, the amount of amniotic fluid increases sharply and quickly, literally within a day, or even in a matter of hours. The changes are visible to the naked eye, as the woman’s belly is also growing. The situation is aggravated by the appearance of painful sensations in the perineum, lower back, swelling of the abdominal wall, and finally, a sharp increase in pressure, due to which the fetal heartbeat is difficult to hear.
But in the later stages there is no need to worry about this: acute polyhydramnios is most often diagnosed in the first trimester, which cannot be said about chronic polyhydramnios. It is from this that expectant mothers who are pregnant suffer. How is it characterized?
- Slow and gradual increase in water volume.
- As a result, a gradual increase in the size of the abdomen, which a woman may not even pay attention to.
- Less commonly – swelling in the lower extremities, nausea, abdominal pain.
You may also experience:
- weakness;
- deterioration of condition;
- feeling of heaviness in the stomach;
- shortness of breath.
At this time, you can often hear gurgling in the stomach. With polyhydramnios, he himself reaches a volume of 100 - 120 cm. Many stretch marks appear on him.
If you suspect these symptoms in yourself, you should not put off going to the doctor. Simply because the condition is dangerous not only for the mother, but also for the child. But first things first.
Why does it occur
Modern medicine can name the main reasons for the development of polyhydramnios, but not all of them. In approximately 30% of cases, it is not possible to understand why this happened. Most often, the situation arises when the woman herself is not large (she is small and fragile), and the child she is carrying is a hero. 
But there are other factors, including:
- (leads to the development of pathology in 95% of cases);
- diabetes mellitus (it is the cause in every third case);
- intrauterine infection;
- diseases of the cardiovascular system;
- placental disorders;
- kidney disease;
- gestosis and that same nausea in later stages;
- multiple pregnancy;
- infectious diseases suffered in an interesting position;
- fetal malformations (problems with the central nervous system, decreased excretory function, problems with swallowing).
Few people know that almost before giving birth, a child absorbs up to 4 liters of liquid per day, and so on every day. But there is no need to worry about this, because it is updated every three hours.
Why is it dangerous?
The consequences of the development of polyhydramnios can be disastrous if measures are not taken. First of all, the condition is dangerous for the baby himself, who now becomes more active and risks getting entangled in the umbilical cord.
How else is the condition dangerous?
- Development of late gestosis, if there was none. This happens, for example, if the amount of amniotic fluid increases at 32–33 weeks.
- Premature birth due to early rupture of water.
- Placental insufficiency, which can provoke chronic hypoxia of the fetus and, as a result, a threat to its normal development.
- Complications during childbirth.
It has been proven that polyhydramnios prevents the baby from taking the correct position immediately before delivery. As a result, a diagnosis of “presentation” is made, with which they are sent to the hospital, of course, if the situation does not change. 
Other possible consequences:
- Weakness of labor, which is caused by excessive distension of the uterus. Under such conditions, the placenta may detach prematurely, which will lead to the development of bleeding.
- Prolapse of the umbilical cord at the time of delivery or the baby’s arms or legs, which, on the one hand, will increase the risk of developing injuries in him, and on the other hand, will complicate the work of doctors and prolong the process. In this case, sometimes asphyxia occurs, which in the future can affect mental development. At risk are women who were diagnosed with polyhydramnios at 36–37 weeks.
But the worst thing is that polyhydramnios at any stage, including at 38–39 weeks, can cause the appearance of intrauterine pathologies that, at a minimum, threaten the child’s health, and at maximum, his life.
Diagnostics
Polyhydramnios is detected during an additional ultrasound, where the doctor determines the amniotic index, that is, the volume of fluid.
There are standards for different periods. So:
- at 16 – 18 weeks the indicator should be in the range of 73 – 220 ml;
- at 22 – 26 weeks – 89 – 238 ml;
- at 32 – 34 weeks – 77 – 278 ml.
Polyhydramnios is an insidious pathology, so if at 34–35 weeks, when the mother feels great, she is given the upper limit of normal and hospitalization is recommended, she must agree. This pathology must be constantly monitored to prevent something terrible from happening! Remember this!
Sometimes the diagnosis of “Polyhydramnios” is preceded by the diagnosis of “Moderate polyhydramnios”. What does it mean? The presence of a problem and its slow rather than sudden development. That is, the amount of water is increasing, although not as quickly as it could, but there is time to correct the condition.
When the pathology is identified, it’s time to find its causes, because treatment depends on them. Therefore, the mother is prescribed:

Cardiotocography may be prescribed to confirm the diagnosis.
Prevention and treatment
Ideally, therapy is prescribed depending on the identified cause of the pathology. So:
- in case of Rh conflict, immunoglobulins are administered;
- intrauterine infection - antibiotics are prescribed that are approved for women in an interesting position;
- diabetes mellitus – diet and additional therapy to correct sugar levels.
True, due to a third of the unknown causes of pathologies, the question of how to treat polyhydramnios in each specific case is sometimes not even raised, because there is a “universal scheme” to get rid of the problem for sure.
What does it mean? What the expectant mother is prescribed all at once:
- antibiotic therapy with broad-spectrum drugs;
- diet;
- diuretics;
- preparations containing magnesium.
To maintain immunity and improve the general condition of the mother and fetus, vitamin complexes containing vitamins B, C, and E are also prescribed.
As a last resort, at 33–34 weeks, an amniotomy can be performed in case of chronic pathology. This is a procedure in which the bladder is opened to release some of the water. Thus, doctors can protect themselves and the pregnant woman from a rupture, in which the waters recede rapidly, taking with it the umbilical cord or limbs of the baby and jeopardizing his life and health.
In the later stages, at 36–41 weeks, a decision may be made to induce labor.
All these problems can be prevented by planning a pregnancy (this is an examination before conception), undergoing regular examinations, and listening to the doctor’s recommendations.
The baby spends 9 months of intrauterine life in the uterus, as if in a small spa, surrounded on all sides by amniotic fluid. They protect the baby from any shocks and shocks, allow him to freely change his body position and “teach” him how to breathe and swallow correctly. But there may be too much amniotic fluid - and then the pregnancy is at risk, and the woman is diagnosed with polyhydramnios.
Signs of polyhydramnios
“You probably have polyhydramnios, that’s how huge your belly is!”- some pregnant women hear from family and friends. The impression of a “huge belly” may arise due to the physique of the pregnant woman and the position of the fetus.
” However, one of the obvious signs of polyhydramnios is an increase in the girth of the abdomen in the navel area to a meter or more.
- In this case, a woman may experience difficulty breathing, it is difficult for her to eat, she has severe heartburn - this happens due to the very high position of the diaphragm.
- A large volume of fluid, coupled with difficulty breathing, causes weakness, fatigue, severe shortness of breath even from minor exertion, and increased heart rate.
- Abdominal pain appears, the expectant mother subjectively perceives it as “heavy”, “stony”.
- The skin of the abdomen quickly becomes covered with rough stretch marks - the pressure on it increases faster than it can adapt.
- There is noticeable swelling of the abdomen and legs.
” Finally, a fluctuation appears - a squelching sound is heard in the stomach when moving.
None of these signs in itself indicates polyhydramnios, but any of them is a reason to consult a doctor unscheduled for an accurate diagnosis.
Diagnosis of polyhydramnios
The main method for diagnosing polyhydramnios has been and remains ultrasound. To assess the volume of amniotic fluid, the ultrasound doctor calculates the amniotic fluid index. To do this, he mentally draws a vertical and horizontal line in the middle of the uterus and determines the maximum distance from the wall of the uterus to the fetus in each of these four conditional sectors. The sum of the four measurements can range from 5 to 24 cm (some doctors narrow this interval to 8-18 cm) and varies depending on the stage of pregnancy.
Normal amniotic fluid index values

” Acute polyhydramnios is especially dangerous, when the volume of fluid increases sharply literally within a day. The woman physically feels sudden changes, and this is an indication for mandatory hospitalization, even if at the time of the ultrasound examination the amniotic fluid index was on the border of normal.
Chronic polyhydramnios, on the contrary, may not be felt by the expectant mother, who gets used to gradually increasing unpleasant sensations. However, this does not mean that she and the child do not suffer from the situation.
Causes of polyhydramnios during pregnancy
There are quite a few reasons for polyhydramnios; moreover, according to various sources, in 27-60% of cases they cannot be found out. However, there are several common conditions that can cause this pregnancy complication.
Diseases of a pregnant woman
- Some chronic diseases of women that arose before pregnancy cause polyhydramnios. Cardiovascular diseases, kidney diseases and diabetes mellitus require the greatest attention.
- Separately, it is worth highlighting infectious diseases suffered during pregnancy - even a banal ARVI affects the membranes of the fetus, as a result of which the normal rhythm of their functioning is disrupted.
- Features of pregnancy
- Polyhydramnios occurs when there is a Rhesus conflict between mother and child, in the case of a multiple pregnancy (often polyhydramnios of one fetus is accompanied by oligohydramnios of the other), as well as if the size of the fetus exceeds the norm.
Fetal problems
- Since in the second half of pregnancy the volume of amniotic fluid is largely regulated by the baby’s digestive system (he actively swallows amniotic fluid and defecates), any problems in the baby are immediately reflected in the volume of fluid.
- Sometimes polyhydramnios occurs due to gross malformations of the fetus - perhaps this is a kind of natural mechanism for terminating a non-viable pregnancy.
How dangerous is polyhydramnios for a pregnant woman and child?
During pregnancy
- A highly raised diaphragm provokes repeated debilitating vomiting in every third woman with this diagnosis. Paradoxically, polyhydramnios can cause a woman to suffer from dehydration.
- Polyhydramnios necessarily causes late gestosis - every fifth woman with this diagnosis suffers from painful swelling and high blood pressure.
- Due to breathing difficulties, both mother and child suffer from hypoxia - lack of oxygen. In especially severe cases, the child may even die.
- A large volume of amniotic fluid allows the child to move excessively actively - this occurs, and 6% of babies before birth cannot take the correct position - because of this, a gynecologist-obstetrician may recommend.
” Finally, the most dangerous complication is partial or complete detachment of the placenta as a result of excessive pressure of amniotic fluid on the walls of the uterus. It inevitably leads to the death of the fetus - without medical intervention this occurs in 30% of cases.
Polyhydramnios is difficult for the child himself to tolerate- if the cause of this condition is an infection, then it can occur; the child’s central nervous and digestive systems often suffer.
During childbirth
- Polyhydramnios causes premature birth - the fetal bladder simply cannot withstand such pressure from the inside.
- The walls of the uterus are overstretched by a large volume of water and cannot contract normally during childbirth - weakness of labor occurs.
- A sudden outpouring of a large volume of amniotic fluid leads to the prolapse of a fetal arm or leg or umbilical cord loops - an experienced obstetrician can promptly correct them, returning them back to the uterus, but he will only have a matter of seconds to do this.
” Finally, polyhydramnios can cause heavy bleeding during childbirth. Acute polyhydramnios is especially dangerous - it is accompanied by high blood loss during childbirth in half of the cases.
What tests are done for polyhydramnios?
The main method for diagnosing polyhydramnios is ultrasound. But to find out the reasons that led to polyhydramnios, the following tests are performed:
- General blood and urine analysis
- Blood glucose test - to confirm or rule out diabetes.
- Vaginal smear - to identify hidden urogenital infections.
- Blood test for antibodies in case of Rh conflict between mother and child
Doppler measurements and cardiotocography (CTG) are done at least once every 5-7 days to make sure that polyhydramnios does not cause serious damage to the child.
Treatment of polyhydramnios
Depending on the identified cause of the pathological condition, specific therapy for the underlying disease is carried out. However, in any case (including if the cause of polyhydramnios cannot be determined), the doctor may recommend the following treatment.
- Taking multivitamins
- If there is a suspicion of an infectious disease, take broad-spectrum antibiotics approved for use in the second and third trimesters of pregnancy.
- Taking diuretics.
- Medicines designed to improve placental blood supply and the condition of the placenta as a whole.
” Finally, the doctor may recommend amnioreduction - therapeutic and diagnostic amniocentesis, when excess amniotic fluid is slowly removed from the uterine cavity - up to 200 ml at a time.
Depending on how successfully the pregnant woman’s condition was stabilized, the issue of the date of birth is decided. As a rule, labor is initiated at , and the baby is born almost full-term and fully viable. In rare cases of continuous increase in symptoms of polyhydramnios, emergency delivery is carried out at any stage of pregnancy.
” Fortunately, truly dangerous acute polyhydramnios is quite rare - approximately 1 time in 300 pregnancies. Moderate polyhydramnios, on the border of the physiological norm, is diagnosed in every tenth pregnant woman.
This is a fairly common condition, and if you have been diagnosed with polyhydramnios, do not panic or be upset, but be positive and follow the instructions of your doctor exactly!
Prepared by Alena Novikova
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
What is polyhydramnios during pregnancy?
Throughout the entire period pregnancy The fetus is in amniotic fluid (amniotic fluid) in the uterine cavity. The importance of amniotic fluid for the development of the fetus and its safety in the womb is enormous.Amniotic fluid protects the fetus from mechanical influences from the outside (blows and shocks), gives the fetus the opportunity to move freely, takes part in the metabolism of the fetus, and protects the umbilical cord from squeezing.
At different stages of pregnancy, the amount of amniotic fluid is different: for example, at 10 weeks the volume of amniotic fluid is 30 ml, at 14 weeks it is already 100 ml, and at 37-38 weeks the volume of amniotic fluid reaches 1-1.5 liters.
Polyhydramnios is a pathological condition, a complication of pregnancy with an excess of the normal volume of amniotic fluid. Polyhydramnios can develop both in the early stages of pregnancy and in its later period. This complication occurs in approximately 25% of pregnant women.
Amniotic fluid is in a state of constant movement and systematic renewal.
Causes of polyhydramnios
The causes of polyhydramnios are currently not fully understood and not precisely established.The risk group for polyhydramnios includes women in the following situations:
- diabetes mellitus in a pregnant woman;
- infectious diseases (rubella, toxoplasmosis, cytomegalovirus infection, herpes infection); these diseases may have mild symptoms, so they are sometimes difficult to diagnose;
- bacterial infections suffered by a woman before conception or during pregnancy;
- diseases of the cardiovascular system;
- kidney diseases;
- multiple pregnancy (identical twins); Often there is polyhydramnios in one fetus and oligohydramnios in the other;
- large fruit;
- placental tumor or other placental pathology;
- fetal anemia;
- Rh-conflict pregnancy (the mother has Rh-negative blood factor, and the father and fetus have Rh-positive blood);
- violations of excretory function in the fetus;
- pathology of the fetus itself: genetic abnormalities, malformations of the central nervous system, heart, kidneys, gastrointestinal tract.
Women in this group develop polyhydramnios more often than women who do not have these risk factors, but they may not develop it.
In the third trimester, the cause of polyhydramnios may be impaired swallowing function in the fetus. During this period, the child daily absorbs up to 4 liters of amniotic fluid, then excreting it in the urine. Swallowing disorders may be associated with fetal developmental anomalies (cleft palate or upper lip), fetal hydrocephalus, disorders of the formation and development of the cardiovascular system, nervous system, and gastrointestinal tract.
In 30% of polyhydramnios that develop during pregnancy, the cause of this complication cannot be determined.
Forms, types and degrees of polyhydramnios
There are 2 forms of polyhydramnios – acute and chronic.- Acute polyhydramnios – a sharp increase in the volume of amniotic fluid occurs and rapidly increases. Over the course of several days (and sometimes even several hours), the size of the abdomen increases sharply, and pain in the lumbar and groin areas is disturbing. This type of polyhydramnios is typical for early pregnancy.
- Chronic polyhydramnios - the amount of amniotic fluid exceeds the norm, but its volume increases gradually; The woman's condition is usually stable.
- Relative polyhydramnios is not dangerous, but only if the doctor is sure that the pregnant woman does not have any infections. This type of polyhydramnios most often develops with a large fetus.
- Borderline polyhydramnios (also called a tendency to polyhydramnios) - the volume of amniotic fluid is at a borderline level between normal and increased values.
- Idiopathic polyhydramnios - its cause remains unclear.
- Moderate polyhydramnios - characterized by a slight deviation from the normal amount of amniotic fluid and a gradual increase in symptoms. Often, external manifestations of moderate polyhydramnios are completely absent.
- Severe polyhydramnios – the pregnant woman’s belly quickly increases in size, the woman feels active movements of the fetus, as well as pain in the lower back and perineum.
- Mild degree - the volume of amniotic fluid reaches 3 liters;
- Moderate degree – amniotic fluid volume is 3-5 liters;
- Severe degree - the volume of amniotic fluid is more than 5 liters.
Signs of polyhydramnios
 Manifestations of polyhydramnios can be different; they are associated with the pressure of an enlarged uterus on neighboring organs.
Manifestations of polyhydramnios can be different; they are associated with the pressure of an enlarged uterus on neighboring organs. Many of the symptoms inherent in this complication of pregnancy can be regarded by women as ordinary and acceptable signs of pregnancy itself, and not of its pathology.
Symptoms of polyhydramnios may include:
- feeling of heaviness, discomfort and frequent abdominal pain;
- constant feeling of weakness;
- shortness of breath with minimal physical activity (occurs due to the high position of the diaphragm);
- increased heart rate (often sudden);
- severe swelling of the lower extremities, anterior abdominal wall, labia;
- the abdomen in girth at the level of the navel exceeds 100-120 cm;
- Often a woman feels a distinct “squelching” or “gurgling” in her stomach;
- the appearance of a large number of rough stretch marks;
- excessive enlargement of the uterus, inappropriate for the duration of pregnancy;
- decrease in daily urine output;
- increased fetal anxiety;
- difficulty listening to the fetal heartbeat.
- woman's complaints;
- medical examination and examination data;
- vaginal examination data;
- Ultrasound scan data.
- premature termination of pregnancy (miscarriage or premature birth) is observed in 28% of pregnant women with polyhydramnios;
- uncontrollable vomiting develops in 36% of women;
- increased blood pressure in a pregnant woman;
- incorrect fetal position – in 6.5% of women with polyhydramnios;
- umbilical cord entanglement due to excessive fetal activity;
- development of placental insufficiency (30% of pregnant women), and even fetal death;
- fetal hypoxia in the early stages causes a delay in fetal development, in the later stages it affects the child’s nervous system and reduces his immunity;
- malformations of the gastrointestinal tract and central nervous system can also be a consequence of polyhydramnios;
- if polyhydramnios develops after an infection, infection of the fetus may also occur;
- bleeding in women with acute polyhydramnios occurs in 41% of cases, and in chronic polyhydramnios – in 6% of cases;
- Late gestosis affects up to 20% of pregnant women with polyhydramnios;
- premature discharge of amniotic fluid;
- premature placental abruption;
- weakness of labor due to excessive stretching of the uterus;
- prolapse of the umbilical cord or parts of the fetus (legs, arms) during childbirth.
A rapid increase in symptoms can even lead to uterine rupture.
The symptoms of chronic polyhydramnios are not clearly expressed, they increase gradually, and the woman manages to adapt to these changes. Diagnosing chronic polyhydramnios can be difficult.
Diagnosis of polyhydramnios
 When establishing a diagnosis of polyhydramnios, the following are taken into account:
When establishing a diagnosis of polyhydramnios, the following are taken into account:Complaints of a pregnant woman with polyhydramnios boil down to general malaise, shortness of breath, a feeling of heaviness in the abdomen, pain in the lower back and perineum.
A medical examination and examination reveals pallor of the skin and a decrease in the subcutaneous fat layer on the pregnant woman’s abdomen; often the venous network is clearly visible on the abdomen. The abdominal circumference does not correspond to the gestational age (exceeds it). When palpated, the uterus is sharply enlarged, it has a spherical shape, and its tension is felt. The fetal heartbeat is difficult to hear, and the fetus itself easily changes its position when palpated. Individual parts of the fetus can be felt with great difficulty.
A vaginal examination reveals a shortened cervix with a slightly open internal os, through which a tense amniotic sac can be identified.
Ultrasound scanning allows the doctor to clarify the gestational age, determine the expected weight of the fetus and the volume of amniotic fluid, and also, using special calculations, determine the so-called amniotic fluid index (AFI)
AFI - amniotic fluid index

This index is measured in millimeters or centimeters, and is calculated by special calculations based on ultrasound data. The amount of amniotic fluid, and therefore the IAF, changes almost daily.
Some researchers consider 6-24 cm to be normal values for AFI, others – 8.1-18 cm. With polyhydramnios, these numbers increase.
There is also a table of normal AFI values for each week of pregnancy. With this table, the doctor can compare the data obtained from the ultrasound scan.
Consequences of polyhydramnios
Despite the importance of amniotic fluid for the normal development of the fetus, an increase in the amount of amniotic fluid is an unfavorable factor affecting the course of pregnancy and the fetus itself.The earlier polyhydramnios occurs, the more fluid accumulates in the uterine cavity, and the higher the risk of complications.
The consequences of severe polyhydramnios are quite serious:
Moderate polyhydramnios, although it has an effect on the fetus, gives a greater chance of pregnancy to term and spontaneous childbirth. Its consequences are rarely severe.
Childbirth with polyhydramnios
From the moment the development of polyhydramnios is established, a pregnant woman should be under constant medical supervision.With mild and moderate degrees of polyhydramnios, they try to continue the pregnancy until the physiological term of its completion.
If severe respiratory or circulatory disorders occur, early delivery is indicated.
Birth with polyhydramnios is often premature. The amniotic sac ruptures suddenly, which entails a copious outpouring of amniotic fluid. It is such an abundant outpouring of water that can lead to prolapse of a fetal leg, arm, or umbilical cord and be an indication for cesarean section. Early rupture of amniotic fluid leads to weakening of labor; contractions may be completely absent.
Excessive stretching of the uterus can lead to premature placental abruption or heavy bleeding in the postpartum period. And the incorrect position of the fetus (transverse or gluteal), which it can assume with polyhydramnios, can also serve as an indication for surgical delivery by cesarean section.
To avoid serious consequences during childbirth when amniotic fluid ruptures, an early puncture of the amniotic sac is performed. As a result of this manipulation, the amniotic fluid pours out in a thin stream, the uterus gradually contracts, and contractions intensify.
However, in most cases with polyhydramnios, delivery is carried out by caesarean section.
Treatment of polyhydramnios
If pregnancy continues, then it is necessary, if possible, to establish the cause of polyhydramnios and carry out the necessary treatment. As a rule, a woman receives this treatment in a hospital setting.Treatment usually includes broad-spectrum antibiotics (except tetracycline), B vitamins, diuretics, drugs that improve blood microcirculation and uteroplacental blood flow.
Polyhydramnios, detected at an early stage of development, can be effectively treated without consequences for the mother and fetus.
In cases of acute severe polyhydramnios, amniotomy (opening of the amniotic sac) is often resorted to and excess amniotic fluid is drained. As a last resort, if the mother’s life is at risk, they resort to termination of pregnancy.
Prevention of polyhydramnios
In order to avoid complications during pregnancy, including the development of polyhydramnios, you should prepare for conceiving a child in advance. It is necessary to carry out all the necessary examinations recommended by the doctor even before the planned pregnancy in order to identify the existing pathology (risk factors) and carry out the necessary treatment.Throughout pregnancy, a woman should visit a doctor in a timely manner, inform the doctor about any changes in her condition and well-being, and carry out all prescribed examinations. A woman’s healthy lifestyle, proper diet, walking in the fresh air and work-rest regime are of considerable importance.