WHEN SHOULD YOU NOT PRESSURE?
With normally established breastfeeding, if the mother is not separated from the child for a long time until the moment when he is able to drink and eat “regular food” in sufficient quantities, there is no need for pumping. If the baby takes the breast correctly (see article) and feeds on demand, there is no need to express after feedings in order to maintain lactation. If the baby does not have enough milk, he will begin to latch on more often (perhaps even “hang” on the chest for several days) and increase the volume of milk from the mother. However, there are quite a few situations where expressing some milk or even pumping your breasts regularly is necessary.
WHEN SHOULD YOU PRESSURE?
Express milk into your baby's mouth to soothe him and encourage him to latch onto the breast;
To alleviate the condition with strong filling with milk or engorgement of the breast, when it is difficult for the child to take a full breast;
Relieve the condition of blocked milk duct or lactostasis;
Feed a child who, for some reason, cannot yet breastfeed (a weak, low-birth-weight child, an illness in the child, a premature baby, breast refusal, a child learning to latch onto a breast with non-standard nipples);
Leave breast milk for the baby or simply maintain lactation while the mother is away or goes to work.
Expressing consists of two stages. At the first stage, you prepare clean dishes for expressing (wash with soap and then sterilize or fill with boiling water for a few minutes and then drain the boiling water), and also prepare yourself. The second stage is actually expressing milk. Hand expression is usually quite effective; if pumping is necessary for a long period of time (for example, the birth of a premature baby who is not yet able to breastfeed, going to work or school), then it makes sense to think about buying a breast pump.
WHY DOES MILK START TO FLOW FROM THE BREASTS?
Milk in the breast is stored in special “milk sacs” (alveoli) located throughout the breast (there are millions of them). From the pouches, channels with milk, milk ducts, lead to the nipple. Closer to the nipple, the ducts merge (like rivers); at the nipple itself there are small expansions of the ducts, which then go out to the nipple in narrow channels. When the baby is properly attached to the breast, he presses on the expansion of the ducts at the nipple (sometimes they feel like small beans to the touch), squeezing milk towards the nipple. Milk flows out of them and runs into the baby's mouth. In order for the expansion of the ducts to fill again, milk must flow from the ducts again. This is not a quick process. However, if the oxytocin reflex is activated, milk sprays out in streams. When does this reflex turn on? When the baby begins to stimulate the nipple, as well as in other situations (the mother hears the baby crying, thinks about the baby), the hormone oxytocin is released. In response to this, the walls of the storage pouches located throughout the breast are compressed, and milk is squeezed out of them directly into the ducts, and from there the flow rushes to the nipple and into the baby's mouth. The calmer the mother is, the more she thinks about the baby, touches him, the more her nipples are stimulated, the better this reflex works. Sometimes a woman herself feels the work of the oxytocin reflex, then she calls it “a rush of milk.” This may be compression or tingling in the breast, tingling in the nipple area, leakage of milk at the moment when the mother begins to think about the baby or feeds him with the second breast. If your baby lifts off the breast and you see milk flowing, this is a sign of an active oxytocin reflex. However, a nursing mother may feel hot flashes only during some feedings or not at all, but the oxytocin reflex will be active. When the baby begins to suck or the breast begins to be stimulated, the reflex turns on, but after a while it stops and the jets weaken. If stimulation continues, the reflex will turn on again (a new “tide” will begin).
HOW TO MAKE MILK FLOW FASTER
In fact, it often only takes a little stimulation of the breasts to get the milk flowing. But some women are helped to achieve larger volumes of expressed milk by certain tricks - often each with their own something. We offer a list of various techniques.
In order for the oxytocin reflex to turn on and the milk that has accumulated to flow from the breast, it is best to relax as much as possible. You are sure that everything is fine with you, you have milk. It is stored in millions of sacs filling your chest. You eliminate any sources of pain and anxiety, forget about them for a while. You can sit quietly in a comfortable position and drink a warm drink (but not coffee). If possible, have someone close to you massage your neck and back, which will help you relax.
Many people find it helpful to look at a photograph of a child or even hear him cry, if possible, look at the child himself or even hold the child in his arms, touching his delicate skin and smiling at him, talking to him. Give free rein to pleasant thoughts about your child. You can warm your chest - for example, put a warm compress on it or take a warm shower. It's a good idea to stimulate your nipples for a while by lightly pulling or rolling them with your fingers - this is a very effective way to trigger the oxytocin reflex.
Sometimes it helps to imagine splashing streams of water, such as a waterfall.
Some women find it helps if they gently pat their breasts with their fingertips or a comb. Some women find it helps if they gently rub their fingers across the breast towards the nipple. You can also massage your breasts. Starting from the top, make circular movements with your fingers on your chest for a few seconds and then move in a circle. Press as much as necessary for a pleasant sensation. Massage in a spiral around the chest towards the areola. After this, you can make light strokes from the edge of the breast to the nipple, along the entire circumference of the breast.
Here are examples of breast massage before pumping - video http://www.youtube.com/watch?v=oXtlqY002s0, description (another massage method, also very effective) http://www.mleko.ru/index.php?pid=4
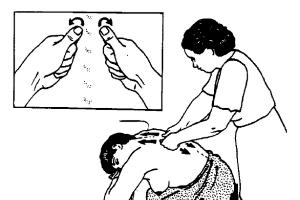
One way to prepare is to massage mom's back before pumping. In this case, you sit down, lean forward, fold your hands on the table in front of you and lower your head on them. The chest and back are bare, the chest hangs freely down. Your assistant clenches his hands into fists, with his thumb facing out, and with his thumb begins to make small circular movements, rubbing his back along the spine on both sides from top to bottom, from the neck to the shoulder blades for two to three minutes.

After the preparatory procedures, you can proceed to pumping.
HAND EXPRESSION
Sit or stand comfortably, holding the vessel close to your chest.
Place your thumb on TOP of the areola (peripapillary circle), and your index finger BELOW the areola opposite your thumb. The remaining three fingers of the hand support the chest.
Apply gentle pressure with your thumb and forefinger to your breast as you push them deep into your breast, plunging your nipple into it. Not too deep so as not to squeeze the ducts. Then use your thumb and forefinger to squeeze the area of your breast behind the nipple and areola. You need to press on those same bean-like extensions of the ducts (though they cannot always be felt, but if you feel them, press on them).
Press and release, press and release. The procedure should not cause pain. If the procedure is still painful, then the pumping technique is incorrect.
The milk may not appear at first, but after a few presses it begins to drip. It can flow in a stream if the oxytocin reflex is active.
In the same way, press the areola from the sides to make sure that milk is expressed from all segments of the mammary gland.
Avoid rubbing the skin with your fingers or sliding your fingers across the skin. The finger movements should be more like rolling.
Avoid squeezing the nipples themselves. Pressing or pushing on the nipples does not allow you to express milk. This is the same as if a child sucks only one nipple.
Express one breast for at least 5-6 minutes until the milk flow slows down; then express the second; then both again. You can express each breast with one hand or change them if you are tired. The most effective pumping scheme is 5+5, 4+4, 3+3, 2+2, 1+1
An important condition is that the mother herself must express, because... another person, especially a non-professional, could damage or injure the breast.
An important condition - do not look into the pumping container! Research has shown that you can express more milk this way (without looking into the container).
In the figure, the green arrows show the correct pressure points for correct grip and proper pumping, and the blue arrows indicate a good flow of milk. By pressing at the base of the milk storage tanks, we squeeze the milk out of them. Incorrect pressure points are shown in red; they correspond to poor milk flow.

Expressing milk properly takes 20 to 30 minutes, especially in the first few days when little milk may still be produced. It is important not to try to express milk in less time.
wonderful animation in the middle of the article! http://breastfed.info/milk-expression-2/
Manual expression video (in English, but there is translation text next to the video) http://new-degree.ru/articles/consultant/handexpression/
Pumping with a breast pump
With engorgement and sore breasts, it can sometimes be very difficult to express milk with your hands. Expressing with a breast pump helps. It is easier to use a breast pump when your breasts are full. It may be less effective on soft breasts. It happens that mothers combine two types of pumping - first, using a breast pump all the way, then with your hands, or vice versa (if the breast pump does not pump well into an overfilled breast).
A breast pump is also useful when you have to express frequently - in this case, if the milk flows normally, you can think about something else while expressing, for example, reading, watching a movie, talking on the phone, which saves time and effort. On the other hand, hands are a more versatile tool that is easy to wash, and which is always with you, in any situation, and does not cost money.
IF THE MILK IS GOING VERY BAD - WARM BOTTLE METHOD
The warm bottle method for expressing breast milk is a useful technique for relieving severe breast engorgement in cases where the breast is very sore and the nipple is very tight, making hand expression difficult. It is used if it is not possible to express milk in any other way, and it is impossible to attach the baby. Once you have pumped a little with the help of a bottle and reduced breast engorgement, you can then express by hand or attach your baby.
1. You will need a suitable bottle:
Made from glass, not plastic;
Volume 1-3 liters, at least 700 ml;
Wide neck: at least 2cm in diameter, 4cm if possible, to accommodate the nipple.
2. You will also need:
A pan of hot water to heat the bottle;
A little cold water to cool the neck of the bottle;
Thick fabric to hold a hot bottle.
3. Pour some hot water into the bottle to start warming it up. Then
Fill the bottle almost completely with hot water. Don't overfill the bottle
Quickly, otherwise the glass may burst.
4. Let the bottle sit for a few minutes for the glass to warm up.
5. Wrap the bottle in a cloth and pour the hot water back into the pan.
6. COOL THE BOTTLE NECK with cold water - inside and out. (If you do not cool the neck of the bottle, you may burn your nipple skin.)
7. Place the neck of the bottle against the nipple, touching the skin around the nipple, and make an airtight contact.
8. Hold the bottle straight. After a few minutes, the entire bottle will cool down and provide a gentle suction effect, allowing the nipple to be drawn into the neck of the bottle. Sometimes a woman feels a suction effect and may move away from surprise. You may need to start over.
9. Warmth promotes the oxytocin reflex, milk begins to flow and accumulates in the bottle. Hold the bottle until milk flows from the breast.
10. Pour the breast milk out of the bottle and repeat the procedure if necessary, or do the same with the other breast. After some time, the acute pain in the breasts will decrease and it will be possible to express milk by hand or breastfeed the baby.
SANITARY REQUIREMENTS OF SOME MATERNITY HOSPILS
In some Russian maternity hospitals, it is forbidden to give a baby milk expressed with a breast pump; only hand-expressed milk is allowed (SES requirements). In this case, it makes sense to first stimulate the breast with a breast pump for several minutes until the oxytocin reflex turns on and milk flows, then manually express the baby, and finally, continue expressing with a breast pump, which stimulates lactation. In order for more milk to come in next time, it’s a good idea to continue stimulating your breasts with a breast pump for a couple of minutes when the milk is no longer flowing. In this case, more milk will come next time.
HOW OFTEN SHOULD YOU PRESSURE?
To establish lactation, if the child after birth for some reason cannot suckle
You need to start pumping as soon as possible. Preferably within the first 6 hours after birth. It may be just a few drops of colostrum at first, or even nothing at all, but this will help your milk supply begin and speed up the process.
Then you need to express as much as possible and as often as the baby would like to eat. At least once every 2-3 hours, including at night. If night pumping is difficult to achieve, allow a night break of 5 hours. If you pump infrequently, there may not be enough milk.
To maintain milk supply
Pump at least once every three hours
To increase the amount of milk if it turns out that you are not expressing enough
For several days, express very often (every half hour to an hour) and at least every three hours at night.
To leave milk for the baby when the mother is at work
Express as much milk as possible for your baby before leaving for work. It is also important to express milk while at work to maintain a sufficient milk supply.
MILK STORAGE
There are many different standards for storing milk. In the maternity hospital you will hear some numbers, from the pediatrician - others, from friends - others. In particular, in a maternity hospital or hospital, the requirements are usually increased and it is advisable to consume milk as soon as you express it, i.e. the whole process should take no more than an hour. At the same time, at home the requirements are much less stringent. The fact is that breast milk contains protective antibodies that prevent bacteria from multiplying, even if the milk is outside the refrigerator. A scientific study published in 1987 in the International Journal of Childbirth Education found that milk expressed in a clean (but not sterile) container and left at room temperature (19-22 degrees) contained approximately the same amount of pathogens after 10 hours. bacteria, as much as milk placed in the refrigerator for the same 10 hours. However, there are few mothers so brave who leave milk out of the refrigerator for 10 hours. But, having read about such a study, you, having expressed milk with soap-washed hands into a clean, soap-washed and thoroughly rinsed container (for a full-term baby and at home and not in a hospital), will not worry that the milk will sit for 2-3 hours without a refrigerator. You can leave it in the refrigerator for a couple of days, or freeze it for longer. A very detailed article about storing milk from the site http://lllrussia.ru/hranenie_moloka/. There is a detailed article on our website: "" about breastfeeding for working mothers who pump regularly. The following numbers are given there
In summer in a room (cooled by air conditioning) – up to 6 hours
In winter in the room - up to 10 hours
In the refrigerator - not in the door, up to 5 days
In a cooler bag with ice – 24 hours
In the refrigerator freezer - not in the door, 3 months
In a separate freezer (deep freezer) - 6 months or more
References
Back to
leonika (mother of twins) about pumping
from the forum forum.materinstvo.ru
At some point during our feeding, I decided that I needed to freeze the milk just in case. For this reason, a breast pump was rented. This is where the fun began. Medelovsky two-phase breast pump. I began to express and began to worry - it was impossible to express more than 80 grams. I’m already starting to get nervous, wondering how many times I need to apply them so that they eat the norm. And I understand that it doesn’t work out. They don't eat that much. I’m thinking about where to freeze it to feed the children. I’m sitting in the bathroom, pumping, at first I’m all upset, and the milk is flowing like shit, and then I think why am I so unhappy, look at how beautiful, smart my daughters are growing up, I imagined how we’d go with them to the sea to relax, and then to grandma, and then to Bali or Cuba in general, it’s not just milk that started flowing, it just burst - 170 grams, 3 flushes in 29 minutes, my eyes popped out of my head - I’m a super milky nurse, I just need an approach to my breasts. It’s like in sex, some people need romantic interlude, while others don’t, probably my breasts need romantic interlude. I then checked the feeding of the girls. If I was in the mood, there could be three hot flashes during one feeding, and for the first time I saw that the girls began to choke on milk. Then I noticed that one breast responded more easily to hot flashes. I have each breast for each child. Clemie tried to feed the first one, then three flushes were guaranteed; it didn’t work out so well on Angelina’s breast, but she didn’t complain. To be honest, I stopped feeding at the computer, as it clearly reduced the number of hot flashes. They helped a lot when I was very tired of taking their first photos from the maternity hospital. And as for how much they eat now with complementary feeding, I understand that I’m not fattening pigs, well, sometimes the child doesn’t want to eat, well, we don’t eat 200 grams of porridge, and sometimes we don’t eat 150, and sometimes when our teeth hurt and we don’t want to breastfeed, but in general They look good, healthy, but I don’t even look at the norms, I see them and see that everything is fine with them.
In my opinion, feeding is affected by stress, fatigue and excessive demands on oneself and children. As soon as you understand that in any case the child will not die of hunger, you can tune in to a positive mood, and you will allow the child to eat as he wants and if he needs to, give him the opportunity to starve, letting go of your suspiciousness will immediately become easier.
does not work...
I began to notice that my son did not have enough milk :-(
Yesterday I sucked both breasts under frequent feeding before bed. After 4 hours he woke up hungry, I feed him, but there is almost no milk in my chest. 4 hours later I woke up hungry again. How to increase milk production?
Today after feeding I expressed the drops that were there. It’s already been 3 hours, and my chest is confused. What to do?!
and my chest is empty
Hello Tatiana
The fact is that visual breast filling usually occurs only in the first weeks. After this, the breasts are no longer heavy, soft to the touch, but still contain a lot of milk. If you still want to increase your milk supply, it usually helps to feed more often (for example, once every 2 hours or more) at each feeding.
Often there is actually enough milk, but it seems that there is not enough. The "" collection contains a lot of information on this topic. I hope you find something useful.
If my answer is not informative enough, please write more specifically - how much the baby is gaining, how often he feeds during the day and how often at night, how you alternate breasts, and so on.
Pumping
Good evening! Please tell me, I can’t find information anywhere on the correct accumulation of milk, I doubt whether I am accumulating it correctly..? Those. Can I express milk into a breast pump, then pour it into a bottle, put it in the refrigerator, repeat the same thing next time and pour the milk into the previous milk? I just pump 50 ml. Is this milk accumulation correct?
milk storage
Hello. As far as I know, you need to combine cold milk with cold milk. If you have expressed warm water, it is better to cool it in the refrigerator and then combine it. In general, do you store this combined milk for a long time?
Hello, please tell me
Hello, please tell me how the breast pump should fit to the breast and how everything should happen there. I just can’t learn how to express properly, either manually or with a breast pump, at first there are 2-3 streams, then nothing and it even hurts. Maybe my breasts are not standard and nothing suits me?
correct position of the breast pump
Hello. The breast pump should be positioned so that the funnel is clearly in the center, with the nipple in the very middle. It must fit tightly to create a vacuum. It shouldn't hurt!
In order for milk to flow, a rush must begin - this is exactly what is mentioned in the article above. When the tide is high, there are streams. The duration of hot flashes varies from woman to woman; Usually, when a woman has been nursing for some time and the milk comes quickly, the rush lasts at least a few minutes. After this, the jets dry up, after some time a new tide begins and the jets appear again.
Please tell us whether you are breastfeeding your child, and if so, how the child eats. Perhaps you simply cannot “turn on” the tide. when you express artificially.
In general, there is a large psychological component in pumping (for example, actively breastfeeding women often experience a rush when they hear a baby crying, or even think about the baby, and have not fed for several hours) - and without any breast pump))) and vice versa, with artificial pumping it can little to come out, this is not uncommon. It also happens from time to time that the breast pump does not fit. Sometimes you can find the right size funnel, sometimes not.
So if you need help, please write in more detail about your situation.
lump in the chest
On the lower left side of my chest I noticed a lump the size of a plum. I tried to strain my breasts, after 2 days the lump became smaller, like a bean, but it did not disappear. It already hurts to press the seal. tell me how to get rid of it? no temperature. I tried to give it to the child so that he could “eat it”, but it stayed that way. How long after breastfeeding should you express your breasts? I feed every 2-3 hours. baby is 1 month old. I will be grateful for a prompt response
hello Galina, situation
Hello, Galina, the situation is quite alarming. If you are in Moscow, contact Karina Oganesyan.
If not, you need to contact a GW-friendly specialist who could help you. Optimally, contact an AKEV consultant to refer you to a doctor. You may be asked to do an ultrasound or puncture to determine the nature of the contents in the lump (milk or pus?)
The seal is always there, does it ever disappear? Have you recently had a fever? redness in the chest?
Hello! I'm through
Hello!
In a few days I need to leave my baby with dad for 4-5 hours, he is completely “on tit”. Please tell me how much milk I need to leave for them so that the child does not cry from hunger. Baby is 4 months old
Hello. The question is:
Hello. The question is: when filling the breast with milk, in the center of the breast (in the area of the milk ducts and ducts) when pressed, can it hurt, or is it some kind of disease? After feeding, the pain disappears, literally two days ago I finished ultrasound treatment of this breast (there was a lump on the side - everything went away).
The baby takes only one breast.
Good evening.
My daughter is 1 month old, I have been feeding her with only one breast for the whole month, because... On the second breast she does not like the nipple (inverted). I constantly express this *unloved* breast with an electric breast pump. Now one breast is twice as big as the other! Considering that my daughter has to eat more and more milk per feeding, I conclude that this difference will only increase. I don’t want to give up breastfeeding, but I also have absolutely no desire to turn myself into a Frankinstein! Tell me, if I stop breastfeeding my daughter and only use a breast pump and bottle-feed her, will the milk remain or is constant stimulation needed by the child? Maybe you can advise something in this situation.
Hello. Specify
Hello.
Please clarify, do you give your baby expressed milk? If yes, from what source?
In fact, the vast majority of women have different sizes and volumes of milk in their breasts. However, noticeable differences are less common; usually during feeding this happens when the baby eats milk from only one breast. Such mothers often write that after finishing breastfeeding, breast size evens out after some time. However, even during feeding, you want to have breasts of a similar size, so, of course, I understand that you would like symmetry, especially since there is milk in both.
When pumping, you are likely to be able to express less milk than when breastfeeding, because... The breasts are noticeably smaller. This means that if you stop feeding completely, it is unknown whether the baby will have enough milk. In addition, with pumped feeding, additional problems arise, such as a decrease in the amount of milk due to delayed pumping, menstruation, illness, refusal to pump at night, and so on. Increasing the amount of milk expressed is not easy for most women, that is, it is quite a serious burden.
Since your baby is still small, there is usually a good chance of breastfeeding at this age. Is it possible for you to invite a lactation consultant? It is quite possible that she would have helped to place the baby on the second breast. It often helps to form a fold from the breast, shift it from breast to breast (especially when half asleep), and choose a suitable position for feeding.
In any case, to equalize the size, you need to empty the smaller breast more. This is best done by a child; Before your baby takes that breast, it's best to pump more often. It is often possible to express more during milk flow, i.e. during feeding from the first.
You might find some of the following links useful
Thanks for the answer! Consultant
Thanks for the answer!
The consultant has already been invited, the postures and correctness of application have been checked. If there is a chance to straighten everything out without taking it off my chest, then I’ll do it! I freeze expressed milk)))
What city are you in? Child
What city are you in? The child is small, the consultant should help at this age.
In your case, the child lost the habit in a few days, and perhaps became offended that there was no breast, and stopped taking. Many women find the nest method helpful, i.e. carry the baby in your arms, sleep together.
I don't know how acceptable this is for you? Write please
Good evening! Daughter (2 months)
Good evening!
The daughter (2 months) fell in love with the right breast, sucks it well, the flush comes immediately after the start of sucking and then the flushes are regular as the sucking progresses. Once I counted 7 in 25 minutes. Those with an oxytocin reflex should in theory be fine.
She sucks the left breast reluctantly, sometimes cries (in different positions). After rocking and calming, he begins to suck and falls asleep while sucking. Tides are very rare. Always only after prolonged sucking, after 30 minutes and with a small number of sips, when the baby is already sleeping and sucking. Once only the tide was at the beginning, at night. I think she cries because of the lack of at least one rush at the beginning of sucking. There is milk in the breast - if I stimulate the nipple area myself, as when expressing, while the nipple is in the baby’s mouth, she sucks and eats sips. But for some reason she doesn’t want to suck it or she can’t. Our latch is fine, we invited a lactation consultant.
In this breast there are only 2 ducts in the nipple: one small, droplet-like; the second is a tight stream that hits a meter. Maybe she can't press hard on the areola, so the milk doesn't come out well when she sucks?
And what could be the reason for the virtual absence of tides? I count hot flashes by characteristic sips - one sip per movement of the jaw.
Could there be any anatomical features?
Hello, yes, everyone
Hello, yes, all women have left and right breasts that differ in volume and size, some have a little, some have more. The problem with hot flashes may be associated with problems with the back, for example, pinching of some nerves. How do you understand that there are no tides? There is no behavior at all, one swallowing, one sucking on this breast, right?
Try feeding from different positions, for example, from under the arm, or in a relaxed position ()
Have you tried compression on this breast? Or, for example, give it when there is a high tide in another (usually this is more or less simultaneously)?
The baby sucks not only due to compression of the areola, but also due to the vacuum. Does she have any extraneous sounds while sucking? Clicks, smacks?
There are no clicks or clatters, and
There are no clicks or clatters, and the consultant looked at the grip - it’s ok.
Yes, on the left breast there is practically no behavior at all, one sip, one sucking movement. The last time was probably a week ago, and always about 30 minutes after the start of sucking. I myself can express from 20 to 40 ml from this breast - immediately after I start pumping, without a rush (I think, without a rush).
I tried different positions, it didn't help.
In a dream, I first gave the breast with hot flashes so that it would suck out three hot flashes, then quickly changed it to this one - the child immediately begins to push, as if she was having a hard time sucking, grunting appears, tries to push off with her legs from my legs - as if she was straining a lot. As a result, she switches to small sucking movements and sucks herself 2-4 throats every 5 minutes.
With compression, small sucking movements are activated. But the “one movement, one sip” behavior still doesn’t exist.
The child is gaining little weight - in the first month 500 grams from the minimum, in the second - 380 grams, so I worry that the breast is on duty for the prescribed 1.5-2 hours without hot flashes - my daughter suffers, sucks somehow, sometimes even normally in her sleep, but she obviously drinks much less milk than from the other breast.
He writes normally.
“strong” breasts will be more stimulated and produce more milk. some generally feed the child with only one breast... (in this case, some asymmetry may occur, which for the most part goes away after feeding is completed). When feeding from a weak one, perhaps it is worth using compression every time? If you switch to it 30 minutes after the start of feeding from “strong”, will there still be no flush for another 30 minutes?
Apparently, you need to try everything to stimulate weak breasts during feeding. Maybe try to pump before feeding? Does this somehow speed up the flow of milk? or during feeding.
This happens (very different breast behavior), incl. for back problems (signals arrive in different ways). Also maybe after 30 minutes of sucking the latch changes? Watch your child.
20-40 ml is not so little, how long does it take you to express it? Are you sure. that there is no tide? How did you understand this - only drops come?
Good afternoon, I thought
Good afternoon,
I counted my peees several times - there were more than 12.
I express 20-40 ml in 10-15 minutes. I've been thinking a lot these days and am increasingly inclined to believe that there are hot flashes in a weak chest, but it cannot suck them out - there are only 2 ducts, one always has droplets, and from the second a very thin, tight stream flows under great pressure (it can only be seen if you look closely). Maybe it’s physically impossible to squeeze milk out of such ducts into one sip, since they are narrow? There are 4 streams from the second breast, thicker and not tight at all.
The child is still small, there is no routine, we have about 15-20 attachments per day, 5-7 of them at night. Almost all sucking (on any breast) ends in sleep after 20 minutes. At the same time, she can sleep while sucking for an hour. At what point in this case should you offer the second breast? How can you tell if your breasts are already empty? She doesn’t demand a second one even in the evening, she doesn’t cry. If there are whims, then immediately after application, after 10-15 minutes he sucks normally, after 20 he dozes or sleeps.
In general, I understand, I’ll try to alternate more often, and look at the gains. Thanks for the help!
Hello, 12
Hello, 12 urinations is an average number, even lower than average. Some children gain well at 15 pieces, some at 20. Everyone has a different volume of one “pee”. Our main criterion is weight gain.
You probably shouldn’t focus on the presence of hot flashes, just try to feed more in volume. A baby can suckle inactively for an hour and suck out very little...
If possible, see the increase weekly or even once every 3-4 days. Based on these figures, it will be possible to guess what will happen in a month and make adjustments. In the first month your gain was higher, maybe something was different in feeding?
At 1.5 months there was weight loss
At 1.5 months there was weight loss almost to the level of weight at 1 month. In time, this coincided with lactostasis of the milkier breast, although the consultant said that the amount of milk could not decrease so much that there would be such a loss (about 150-200 grams). I weighed myself once a week and noticed the weight loss late. Now I weigh myself every day, although this is not recommended. We are still not gaining weight very well - over the last three weeks, 340 grams; On average, per week it turns out from 90 to 140 grams, depending on the day when you count it - the weight either stands for 2-5 days, then jumps by 20-50-70 grams. And she hasn’t pooped on her own since the maternity hospital, once a week I use a candle or a straw - the weight decreases by 30-50 grams.
Now I try to give one or two breasts at one feeding.
Breasts that are without hot flashes, the daughter sucks poorly - both in behavior and quality. She still gets indignant at a weak flow, as you write - she throws the nipple, arches, but after a while I persuade her, I walk with her in my arms. I can’t stop giving this breast at all, the milk will disappear.
If I do not actively massage the area around the nipple during feeding, then sips rarely occur. She does not always suck milk out of her (although there is not a lot of it there). Sometimes immediately after feeding I can express the same 20 ml. I carried out control weighing 5 times - I ate from 0 to 20 grams.
The milky breast sucks well, but in the evening it becomes capricious in the same way as a weak breast, if there is no second or third flush for a long time. From which I conclude that the appearance of hot flashes in a weak breast would stimulate the daughter to suckle better, which means there would be more milk in her.
Since in this situation the milk breast is our main source of milk, I can’t imagine how to stimulate an increase in milk in a weak breast. I can’t start giving it a cup, because we are already gaining weight poorly - weight loss will begin. At night in her sleep she also sucks it poorly. Maybe I should just pump it all the time? Although during the day I already feed every 1-1.5 hours (with the exception of sleeping outside for 1.5-2 hours) - by the way, for 2.5 months, this is probably too frequent feedings, and indicates a lack of milk?
In short, so far my attempts to establish breastfeeding and normalize the child’s weight have not been very successful. The only good news is that the child looks healthy and she is not restless. If she had cried, as many people write, I definitely would not have been able to stand it and switched to SV.
"Maybe we should just pump her
“Maybe we should just pump it all the time?”
Yes, this is a very good option, but only if you can supplement with this milk from a spoon or cup, without sucking. This is a good stimulation of the amount of milk in this breast, the work of the tides, and the width of the ducts. But you can’t supplement your feeding with a bottle (as well as giving you a pacifier, well, I think you know that))).
"for 2.5 months, this is probably too frequent feedings"
no, there are no such laws. women in tribes feed up to 4 times an hour)))
“Sometimes immediately after feeding I can express the same 20 ml.”
This is what surprises me. Have you tried changing your position while breastfeeding? from=under the mouse?
Honestly, 9 to 1 that the latch on this breast is incorrect, if you can express so much immediately after feeding! And at the beginning the tide does not come, but then it can come - when does the grip change? ;) Are you sure your child doesn't have a short frenulum? Can she put her tongue on her lower lip? Does this happen often?
Have you tried Newman chest compressions? When you squeeze not at the nipple itself, but further to adjust the milk. many women do this intuitively.
I feed the expressed ones from
I supplement the expressed milk with a syringe; we do not use bottles or nipples. The frenulum is fine, the tongue protrudes from the mouth regularly when awake. The grip may not be ideal in terms of symmetry. Especially at night, when I feed lying on my side, stomach to stomach. But the areola is almost entirely in the mouth. I tried relaxed feeding about a month and a half ago, when my tummy was regularly hurting. But she doesn't like to lie on her stomach. Moreover, if the flow of milk is weak, then she needs to strain even more to suck from such a position.
For a little over a week now I have been changing breasts frequently: one or two feedings, changing during feedings - I read an article on this topic on your website. At first glance, the gains have improved and stabilized - we are adding 20-30 grams every day. Previously, we stayed at the same weight for 2-5 days, then there was a jump of 40-70 grams. Let's wait and see.
The day before yesterday I fed well from a weak breast from the armpit, yesterday and today from the cradle - with hot flashes with frequent sips (not many sips, but at least something). I try different positions - sometimes I get better in one, sometimes in another. Today I used compression - the pharynx seems to appear more often.
I'm thinking about buying an electronic breast pump for weak breasts to pump them out. I think if there was more milk, my daughter would drink more.
Thank you very much for your time and advice!
Hello, Daria! Thank you,
Hello, Daria!
thank you for answering))
Different women have different areola sizes, so whether it's all in the mouth or not means different things to different women. An asymmetrical grip and a wide open mouth, the chin resting on the chest - this is most often enough. If the child is not tightly pressed while lying down, depending on the size of the chest, it can help to press the baby with his stomach to you, and even put his legs a little on you, or vice versa, move him away from you so that the head is pulled closer and the grip is better (from below, where the strong the lower jaw should be grasped more than the top).
if you have a manual breast pump, an electronic one will most likely express about the same, the only thing is that you get less tired of it (less manual work), that’s what it’s used for.
Help! Lactostasis
Hello! I was literally tortured by lactostasis. In 2 months of feeding, there were 7 pieces with fever, wild pain in the chest both during feeding and when touched, to the point of tears, at the moment there is lactostasis in both breasts, it is most difficult to strain out the lumps, they are from the armpits at the very base of the breast, I go for an ultrasound. In the first and second months my daughter gained 1300 and 1300 respectively, I feed on demand, I also wake her up at night when she sleeps, I hope the latch is correct (flat nipples), I don’t use nipples, bottles, or pads. The first lactostasis happened 2 weeks after giving birth, I went for an ultrasound, it immediately happened again, it wasn’t for a month and a half, now again, one after another, there is no strength. I don’t pump after feeding (although all doctors strongly recommend it; I’m afraid that there will be even more milk and I’ll have to pump constantly). I'm pumping until I feel better now. The breasts are heavy and dense already 2 hours after feeding; after feeding, milk remains in most cases. My daughter has thrush in her mouth (plaque) - we treat it with soda, I smear my nipples with candida and soda. HELP! This is simply unbearable, I have a very hard time with lactostasis, and I also have to take care of the child (6300 kg in weight).
Mothers most often pump at the time when milk is most plentiful. For example, some people have this opportunity in the morning, others at night. If there is any left over after feeding, and the baby has eaten a lot and is full, then express after such feeding. Some express after, and others during feeding.
Just be sure to try giving your baby defrosted expressed milk. Otherwise, some refuse;) then the supply will not be used for future use.
If it's not a secret, are you going to be away often? For example, once or twice a week, like for an exam, for example, or every day?
3. About the increase - usually in our pediatric tables it costs 600 in the first month, then 800 each. According to WHO, the minimum is 500, but in general it depends not only on the weight, but also on the height of the baby. If you write down your birth weight and height, and your discharge weight, it will be easier for me to check this indicator for you. But you can see for yourself, are there links to WHO charts? just in case. Or are you not considering such options?
How are you doing now, are you satisfied with your feeding? Do you get enough sleep (probably also have night feedings?)? Are you doing what you planned? Is it comfortable and pleasant to feed?
do I need to pump?
Good afternoon, I'm asking for advice.
We are 11 days old. The milk arrived on the 5th day. Feeding on demand. I alternated breasts every 3 hours approximately. The chest filled equally. But one morning, I noticed that one breast was full, but the other was not. And the flow of milk from the smaller breast is very weak. The baby on this breast sucks effectively, swallowing milk for a maximum of 10 minutes, and then falls asleep. Even though there is milk in this breast, he stops sucking it. The other breast is always full. but it doesn't hurt. Just heavy.
Hello, first days
Hello, in the first days there may be too much milk, but now is an important period, it would be good for you to express no less than what the baby needs. Please tell us how many times a day do you pump, what are the breaks, including at night, two breasts or one?
You can also breastfeed after a bottle, this is very good, for example, for sleep. Didn't you do that? Do you use a pacifier, or was it unnecessary?
Hello! Daughter is 1 month old
Hello! My daughter is 1 month 3 weeks old. Because of her illness, I feed her with expressed milk. I feed 110-120 ml every 3 hours, the last time at 24:00 and then at 05:00, I don’t disturb her at night for feeding (we get sick) and she doesn’t wake up on her own. Were born weighing 3010g. height 55cm, in the first month we gained 1 kg, now we weigh 4700g, height 57cm. But the fact is that I have a feeling that the child is not getting enough to eat, I feed her, and after 40-60 minutes she begins to worry, cry, waves her arms and legs, if you pick her up, she begins to look for the breast. To calm her down, I give her a pacifier, she sucks as if she had never been fed at all: (she sleeps poorly during the day (4-5 hours for the whole day) and only on her stomach. I can’t feed more in volume because there is little milk. Tell me, her behavior does it mean that she is malnourished or is it something else? And is it possible to somehow rationalize feeding in our case? Maybe I have “poor quality” milk?
Hello. Am I right
Hello. Do I understand correctly that it is impossible to breastfeed or even let your baby suckle?
If so, you can try pumping more often if you want more milk. However, the gains are good, that is, there is enough milk. But it is difficult to understand a child’s behavior without knowing what she is sick with and why she is unable to breastfeed.
Research shows that women have milk of different fat contents and volumes, but this does not prevent children from eating enough and being satisfied. For milk to become of poor quality, the mother must actually practically die of hunger, that is, be in conditions of severe malnutrition. This is because lactation was established thousands of years ago as a very stable and sustainable mechanism for ensuring the survival of young. That is, you don’t have to worry about the fat content and “quality” of the milk; problems only arise in the form of allergies.
Hello, Anastasia. How
Hello, Anastasia.
As I understand it, you need to go for treatment and you are worried about how the baby will be fed, what, and whether he will then breastfeed.
Quite a lot of questions immediately arise.
1) quite a lot of medications are compatible with breastfeeding in one way or another, and even if something that is not compatible with breastfeeding is prescribed, very often you can choose one that is compatible. Unfortunately, doctors do not always know about this, because... It is customary for us not to feed during any treatment, but it does not take into account that if you do not feed, then there is a risk of abandonment of the breast, a decrease in milk supply, which is more harmful to the child than milk with a small amount of medicine compatible with breastfeeding. Now this concept is being revised, because It became clear that it is better when feeding is not interrupted.
2) pumping - of course, this is very individual. Women often have the best time expressing milk at night and in the morning. Sometimes they even pump before feeding, because it’s still impossible to pump everything, and the baby will still end up with enough milk for himself. In addition, there is another good option - when you feed on one breast, express the second. By the way, do you usually feed one at a time or two at once? As it turns out?
3) some women are also considering the option of going somewhere with the child together, so as not to be separated. After all, the child will miss not only milk, but also his mother. However, if the baby stays, he will be bored and perhaps you can think in advance whether he knows the person with whom he is staying well, whether the baby agrees to drink from the container from which he will be fed - this could be a cup, a spoon, etc. bottle. They don't always just bottle feed. How will the baby calm down, does he suck on the pacifier, or maybe to calm him down, they will rock him, carry him in his arms, or give him a clean finger to suck (they do this too, especially since the finger is more similar to the breast than the pacifier, so children then take better breast). I have a selection of useful materials on this topic:. And an article on this topic. Some even leave some things that smell like mom so that the smell will calm the baby.
Please tell us what you think about these questions?
Expressing breasts at the birth of a premature baby
Good afternoon I would be very grateful if you could help with advice.
At 32 weeks of pregnancy, premature birth occurred, the baby is in the premature babies department, feeding through a tube. On the 3rd day my milk “came”, in the maternity hospital they told me to express one breast every 3 hours, including at night. I still do this, and I can express 50-60 ml from one breast with a breast pump. Feeding the baby with milk is possible no earlier than after 2-3 weeks. Now I want to start freezing milk and I’m puzzled by the following questions:
1. Is it not enough to express milk from one breast at a time? (a week has passed) or should I shorten the intervals between pumping?
2. Is it enough to express only one breast every 3 hours or should I express both at once?
3. What pumping schedule would you recommend for my situation?
Every mother knows how much benefit breast milk brings to babies, and especially newborns. The most important advantage of this type of feeding over artificial feeding is the activation of the baby’s immune forces. Breast milk is also completely sterile and is always heated to the right temperature, which greatly simplifies feeding the baby while traveling and outside the home in general. In addition, breastfeeding helps a new mother quickly recover after childbirth and significantly strengthen the emotional bond with her child.
Due to the inexperience of young mothers, it happens that breastfeeding brings a lot of disappointments instead of pleasure. Milk does not come, or there is very little of it, cracks in the nipples do not go away, or the child flatly refuses to take the mother’s breast - there can be many reasons, they become especially relevant in the baby’s first month.
To solve any of these problems, women often start pumping their breasts. It is worth noting that modern doctors advise not to overuse pumping, they recommend simply feeding the baby, following not the clock, but its requirements. In this case, the mammary gland will produce exactly as much milk as the baby needs.
At the same time, in order to help herself during inflammatory processes such as lactostasis and mastitis, a woman should express breast milk until the inflammation goes away. Soon the baby will begin to empty the breast during each feeding and the likelihood of illness will be reduced to a minimum. As a rule, this will take a month while lactation is established.
It is important to know when to stop
Many young mothers are concerned about the question: how long to express full breasts to avoid congestion? A couple of decades ago, experts answered this question unequivocally: to the end, so that the breasts become completely empty. Today their position is not so categorical: it is recommended to express the breast until it feels comfortable, so that the feeling of fullness and distension disappears.
If you adhere to the “to the last drop” rule, breast milk will begin to be produced with redoubled force, and there will be more of it than one baby can suck. With a high degree of probability, such tactics will lead to congestion in the chest.
How to prepare and express milk

Pumping itself is not pleasant for every woman. In order to overcome discomfort, you need to create a favorable environment: calm music helps some, cold tea helps others, many mothers also recommend back massage... In other words, as many women as there are, there are as many ways to deal with unpleasant physiological sensations.
By the way, it’s worth trying to express breast milk both with your hands and with a breast pump: there are approximately equal numbers of adherents of both the first and second methods. True, in the case of a breast pump you have to put in less effort, especially if the device is electric.
If the baby quickly and actively sucks the breast, you should not buy a breast pump, but if the child is not gaining weight well and sleeps a lot, the device will not be superfluous. As for the question of how long the procedure will take when expressing by hand and with a breast pump, the answer is the same: it will take approximately 15-20 minutes.
Secrets and subtleties of manual expression
Before expressing milk, you need to wash your hands well using antibacterial soap, and find a suitable container (for example, a bottle) with a wide neck, boil it well and place it near the breast. After this, you need to start the pumping procedure with two fingers: place the thumb above the nipple, the index finger under it, and then press on the areola on both sides. Pressing should be alternated with relaxing the fingers. When expressing, you need to carefully ensure that there is no pain. If they occur, the tactics were chosen incorrectly and need to be changed.
If the actions are correct, milk will drip from the breast, and if the ejection reflex is active, it will flow. After the flow decreases, you need to pump both breasts in turn for another 3 to 5 minutes to make sure that there is no excess milk left in any part.
It happens that the breast becomes engorged, soreness appears in it, the nipple becomes tight, and it is completely impossible to express breast milk. In this situation, you can use the pumping method using a bottle.
You must first pour hot water into a sterilized bottle, wait and pour it out. After the neck has cooled (ideally, its diameter should be approximately 3 cm), it must be tightly fixed to the areola of the nipple. After a couple of minutes have passed, it will retract into the bottleneck and milk will drip into the container. To avoid damage to the nipple, you will soon need to remove the bottle and express breast milk into a regular container.
Often mothers are interested in how much and under what conditions to store expressed milk. Breastfeeding experts answer this way: in the refrigerator - 4 days, and in the freezer - up to 4 months.
Frequency of the procedure
As for how many times a day to express, this is a controversial issue. So, with the arrival of milk, and with it a feeling of fullness in the breast, it needs to be expressed for 1-3 days, 1-3 times a day.
If the newborn is separated from the mother (this is still practiced in some maternity hospitals), after each feeding for an hour, missed by the child due to sleep or refusal, both breasts are expressed in turn for 10-15 minutes.
It is worth noting that when milk comes in and lactation is established, you need to gradually stop expressing your breasts, reducing the duration and number of procedures. This usually occurs within the first month of a baby's life, and it will take about a week to completely stop pumping.
So, until the baby is one month old and normal lactation is established, you may have to resort to pumping. However, doctors advise not to delay abandoning this procedure, so as not to provoke the development of inflammatory diseases associated with excess lactation.
How long should you express breast milk?
Almost every mother during the period of breastfeeding sooner or later has to deal with pumping. Even if she is solely committed to breastfeeding, anything can happen. When starting this procedure, it is important to find out how to express breast milk correctly. It is better to prepare and practice in advance so as not to comprehend the basics of this science in a hurry, otherwise you can damage your breasts.
Do I need to express colostrum?
Expressing milk is a common and long-debated question, but some mothers are also concerned about more unusual questions, for example, should I express colostrum?
The answer to this question is not entirely clear. If mother and baby are healthy, close together and committed to breastfeeding, no one will need to pump. Colostrum is produced in optimal quantities, which does not burden the baby’s gastrointestinal tract, but supports his strength.
Expressing colostrum in the first days may only be necessary in a few cases:
- the baby was born premature or weak and cannot breastfeed. Colostrum is offered to him on a spoon or through a pipette;
- the mother cannot feed the child for some time after childbirth - due to anesthesia after the CS or illness. Then, you need to express colostrum with your hands to start lactation;
- with severe jaundice in newborns and prescribed phototherapy;
- with a special scheme for caring for a low-weight baby.
Some mothers begin to produce colostrum during pregnancy. In this case, there is no need to express it either - this will only aggravate the problem. At the same time, milk after childbirth, or more precisely, its quantity, does not depend in any way on the quantity.
Is pumping necessary?
Previously, expressing milk was considered a prerequisite for maintaining lactation, and this made sense - mothers fed their babies according to a schedule, and this caused a cessation of milk production. It was possible to maintain lactation only with additional regular pumping.
 Today, WHO and AKEV experts answer the question of whether it is necessary to express an unequivocal answer - no! This procedure is used only in extreme cases when there is a direct threat to the health of mother and baby.
Today, WHO and AKEV experts answer the question of whether it is necessary to express an unequivocal answer - no! This procedure is used only in extreme cases when there is a direct threat to the health of mother and baby.
Dr. Komarovsky believes that a healthy mother with normal lactation does not need pumping. However, he emphasizes that today there are few women with normal hormonal levels, whose body will normally react to the remains of milk in the breast after feeding. It often happens that in response to this, the body “curtails” lactation, believing that there is too much milk.
AKEV specialists are confident that this situation can be corrected by natural feeding without additional pumping. If you make a little effort and offer your baby the breast more often, lactation will improve in a few days and reach the required level of lactation. In any case, if there are no health risks, the mother herself decides whether to express or not, based on the advice of the pediatrician and her own goals.
Do I need to express milk after each feeding?
Based on the opinion of the World Health Organization and AKEV consultants, we can say that women do not need to pump after each feeding unless there is an extremely serious reason for this.
Waiting after feedings can provoke the development of hyperlactation and, as a result, constant congestion or even mastitis. The child simply will not cope with such a volume of milk - he does not need it.
If the mother’s milk supply is low and the baby is malnourished (this is noticeable by weight gain), you should first of all try to strengthen lactation by putting the baby to the breast more often. Nature has provided for all situations, and within a few days the body will adapt to the child’s needs. According to WHO, breastfeeding after breastfeeding to enhance lactation can only be used as a last resort.
Should I pump my breasts before breastfeeding?
In the past, it was often recommended to “pump” the breasts before breastfeeding in order to develop them. Modern breastfeeding consultants are of the opinion that there is no need to express the breast before feeding - if the mother and baby are healthy, they were not separated after childbirth, and the mother does not take harmful medications. A healthy baby is quite capable of independently stimulating the mother’s milk production.
When should you really express milk?
There are several situations when expressing milk is necessary to maintain the health of the mother or baby:
- during stagnation (lactostasis), if the baby cannot cope on his own;
- during the mother’s illness, if medications harmful to the child are prescribed. At this time, the baby is usually switched to formula, and the mother regularly expresses milk to maintain lactation, imitating the baby’s feeding regimen;
- at the birth of a premature or weakened baby, when he cannot suckle on his own. Feeding expressed milk will be a much better option for the baby than formula;
- When the breast is overfilled with milk (“stone breast”), the nipple may become deformed and flattened, then the baby will not be able to latch on and eat normally. To make the task easier for him, the breast is pumped a little - until the nipple “appears”, then the child can cope on his own;
- to preserve milk supply. If you are planning a long separation from your baby (going to work, a session, traveling on business for the whole day), you can express it into a bottle in advance after and between feedings and freeze it by hour X.
Many mothers are interested in the question of whether it is necessary to express milk when stopping lactation. If breastfeeding ends naturally, breastfeeding occurs gradually, the demand for milk is reduced and the body, accordingly, reduces its production. In this case, there is absolutely no need to express - everything happens very smoothly and without any unpleasant sensations for the mother.
In the case when weaning is carried out abruptly, for example, due to the mother’s illness or other circumstances, the body needs much more time to adapt, and the mother may suffer for some time from the unpleasant consequences of refusal - breast fullness, pain in the breast, or even mild inflammation.
If possible, such a sudden weaning should be smoothed out as much as possible - gradually (once a week or at least every 2-3 days) by removing one of the feedings and replacing it with a mixture or other food.
If this is not possible, you will have to pump. The main thing is not to empty your breasts until they become soft - this will only stimulate the production of prolactin. When you stop breastfeeding, you can express milk only until you feel relieved. If you don't pump at all, stagnation, lactostasis, or even mastitis can form.
After pumping, you can apply a cold compress or a cold cabbage leaf to your breasts. They are good at removing incipient inflammation and relieving the feeling of fullness in the chest.
By hand or breast pump
You can express milk either by hand or with a breast pump. Each mother can choose the most comfortable method for herself, since both have their own advantages and disadvantages:
- expressing breast milk by hand is available to every mother and does not require any extra costs or additional space;
- in some situations, you can express only with your hands, for example, with severe swelling of the breast (“stone breasts”);
- Expressing breast milk with a breast pump is a little faster than expressing it manually. But at the same time, most devices are most effective with full breasts, and from soft breasts they express milk worse, and the mother has to finish their work with her hands;
- The use of breast pumps is prohibited if the skin of the breast and nipples is damaged.
- Any pumping - by hand or with a breast pump - must be preceded by a light breast massage, which will cause a flow of milk.
If a mother pumps rarely, from time to time, the manual option may well be enough for her. Breastfeeding consultants consider this method more physiological and safe. If you have to store milk constantly and in large quantities, a breast pump will be a good helper, the main thing is to choose the right model.
How to Express Breast Milk by Hand
The technique of expressing breast milk is a very important element of the entire procedure. If the technique is not followed, the results can be disastrous. At best, expressed breast milk will unpleasantly surprise the mother with its quantity, and at worst, it can seriously damage the breast tissue.
Many mothers, having tried to express milk for the first time and received a few teaspoons of liquid in response, come to the conclusion that they have hypolactation, the child is not eating enough and this whole thing urgently needs to be stimulated. However, if a child gains weight normally, the issue here is not at all in quantity, but in the inability to “get” it from the breast without the baby’s help.
Both manual and mechanical pumping require more than just theoretical knowledge. To properly express milk, mom will most likely have to practice for a while. The psychological attitude is also very important - confidence in your abilities and positive results will help you relax.
Preparation
For the pumping procedure to be effective, the mother needs to prepare properly. First of all, you need to wash your hands and chest and prepare a clean container. Then you need to create a tide. You can do this in different ways:
- drink warm tea or any other warm drink;
- apply a warm, damp towel or diaper to your chest;
- hold the baby in your arms (in the first weeks after birth, sometimes just thinking about him is enough);
- the most effective remedy is a light breast massage before pumping;
- You can put the baby on one breast and express the other at this time.
After the onset of hot flashes, you can begin to express breast milk manually or using suction.
For manual expression, several techniques have been developed that increase the effectiveness of the procedure.
Marmet technique
This technique was specially developed for breastfeeding mothers to make pumping easier. Algorithm of actions:
- The thumb and index fingers are located at the border of the areola and the skin of the breast, forming the letter C. The remaining fingers and palm support the breast;
- The index finger and thumb slightly squeeze the chest and move towards the chest, as if grasping the milk ducts. At the same time, they should not slide over the skin, they remain on it and move with it, otherwise abrasions will appear.
- Then the fingers “roll” along the ducts lying under the areola in the direction of the nipple. squeezing it a little.
- Repeat until the milk flows. When the intensity of milk release has dropped, you can move to the second breast or change the position of your fingers by moving them a little in a circle.
 This technique allows you to express breast milk with your hands during congestion, since the fingers, moving in a circle, affect all lobes of the breast and help the lumps to dissolve. At the same time, you cannot exert any special influence on them - kneading, pressing, trying to knead them!
This technique allows you to express breast milk with your hands during congestion, since the fingers, moving in a circle, affect all lobes of the breast and help the lumps to dissolve. At the same time, you cannot exert any special influence on them - kneading, pressing, trying to knead them!
It is important to remember that trying to squeeze milk out of the nipple is pointless, there is no milk in it. Expressing milk by stretching and squeezing the nipple will only work if the milk ejection reflex is strong, although the effectiveness will still be questionable.
Nipple compression method
 Sometimes it happens that a lot of milk has accumulated in the breasts, and the nipples become rough, painful, or completely flattened. The baby cannot latch onto it and help the mother, so the nipple needs to be reshaped.
Sometimes it happens that a lot of milk has accumulated in the breasts, and the nipples become rough, painful, or completely flattened. The baby cannot latch onto it and help the mother, so the nipple needs to be reshaped.
To do this, place all fingers on the nipple and begin to gently press on it for 3-4 minutes. There is no need to move your fingers - the pressure is static. It softens the breasts and allows you to either pump painlessly or attach the baby.
This technique allows you to properly express during lactostasis, reducing breast soreness and getting rid of excess milk. However, with stagnation, the main thing is not to overdo it and strictly follow the rules for expressing breast milk during lactostasis, so as not to worsen the situation.
Warm bottle method
 Another way to soften breasts with lactostasis or excessive tension is the “warm bottle” method. In this condition, manual expression of breast milk is extremely painful, and the baby cannot latch onto the breast. To alleviate the mother’s condition, you need to heat the bottle (neck width is at least 4 cm) with boiling water, and then cool the top part and lubricate the neck with Vaseline. It is applied to the breast, the nipple gradually begins to retract inward and milk drips from it. When the intensity of the jets drops, the bottle is removed.
Another way to soften breasts with lactostasis or excessive tension is the “warm bottle” method. In this condition, manual expression of breast milk is extremely painful, and the baby cannot latch onto the breast. To alleviate the mother’s condition, you need to heat the bottle (neck width is at least 4 cm) with boiling water, and then cool the top part and lubricate the neck with Vaseline. It is applied to the breast, the nipple gradually begins to retract inward and milk drips from it. When the intensity of the jets drops, the bottle is removed.
How much milk can you express at one time?
The amount of milk produced directly depends on the time of pumping. After feeding, there may be very little or none at all, except in cases of hyperlactation. If the mother expresses before feeding, you can get about 50-100 ml of milk. Although this figure is quite individual, a significantly lower result indicates incorrect technique, and not a small amount of milk.
Expressed breast milk should be signed immediately so you know its expiration date. It stores well in both the refrigerator and freezer. Bottle feeding with expressed milk allows the mother to go away on business, entrusting the baby to relatives or dad.
Common difficulties and mistakes
First of all, you need to remember that pumping should not cause pain! If a mother's breasts hurt after pumping or already during the process, it means that she does not follow the technique - she squeezes too much or fidgets with her fingers on the skin.
If milk is not expressed, the reason is the same, incorrect technique. You need to relax, choose a comfortable position and be sure to try again. Giving up pumping because of the first failure is also a mistake.
If you can’t cope on your own, breastfeeding consultants or a pumping service can help. They will show the correct technique and teach the mother to cope with this procedure on her own.
There are many conflicting opinions and beliefs surrounding breast pumping. Sometimes it can be quite difficult to resist the established habits of older generations or common myths, but breastfeeding is too important a process to risk. Mothers need to pump their breasts only in the most extreme cases, and in all other cases, the baby can handle the milk just fine on his own.
There are different ways to feed your baby breast milk. Someone attaches the baby at every call and spends with him around the clock. Some people go to work immediately after giving birth, but the baby is still fed breast milk. Pumping will help give the baby milk in the absence of the mother. Pumping skills will be useful to any woman: after all, there are a lot of situations when this will need to be done.
Why do you express milk?
Expressing milk is the emptying of the mammary glands without the participation of the child. The reasons for pumping may vary. For example:
- You have to pump in the first days after giving birth. For some, it is to “accelerate” lactation, for others, to get rid of excess milk.
- Medical indications. For example, after childbirth, a mother needs to take medications that are incompatible with breastfeeding. Or the baby was born too weak and cannot suck milk on his own.
- If the mother needs to leave for a while, the milk is expressed so that the nanny or relative can feed the baby the usual food.
- Pumping helps minimize the consequences of mother’s “sins.” In particular, many women pump after consuming junk food or drinks. This milk is disposed of. The breasts have to be emptied of milk even after fluorography or a chest x-ray.
- If the baby ends up in intensive care after birth, the mother will have to express milk for quite a long time. Firstly, to maintain lactation, and secondly, so that this milk is fed to the child.
- This procedure is useful during the treatment of congestion, lactostasis, and also during the “winding down” of lactation, after completion of feeding.
- Mothers of twins and especially triplets are forced to pump in order to at least sometimes take a break from feeding.
- You can express breast milk not only for your baby, but also for someone else’s. Donor milk can be sold or given to those who need it.
There are cases when a woman breastfeeds her child for many months or even years, but she is never given the opportunity to express herself. That is, this procedure is completely optional. But for many mothers, pumping helps regulate the amount of milk and gives them some freedom - to go to the cinema, go shopping or just visit a friend. These seeming little things often affect the maintenance of lactation as a whole.
You can express with your hands, on your own or with the help of others (nurse, doctor, husband). There are also special devices - breast pumps. They can be manual (they have a special bulb at the end that needs to be squeezed and unclenched by hand) or electric. The electric breast pump does everything itself. For expressed milk, sterile bottles or special containers are usually prepared.  Test jars are an excellent alternative to expensive milk containers: they are sterile and have a measuring scale
Test jars are an excellent alternative to expensive milk containers: they are sterile and have a measuring scale
Preparation
The process of pumping takes energy and time. To make it as comfortable and safe as possible, you need to carefully prepare.
First you need to prepare containers for milk. Ideally, they should be sterile: use a sterilizer or simply hold them over steam.
If the milk is not intended for the baby, you can express it over the sink or over the table, laying a soft towel on it.
To make milk flow faster, you need to speed up its outflow. To do this, it is recommended to take a warm shower before starting pumping. You can massage your breasts with water from the shower head, directing it towards yourself. The water should be warm and pleasant, and the streams should be soft. After this you need to do a light massage:
- One hand should be placed under the chest, the other on the chest.
- Using circular movements you need to “pass” the entire mammary gland from the ribs to the nipple area.
- If compactions are felt somewhere, you need to massage these places longer.
 Hand movements should be soft so that the massage brings only pleasant sensations.
Hand movements should be soft so that the massage brings only pleasant sensations. Hormones also affect milk flow. To stimulate yourself, you can look at photographs of your baby or think about him. There is no need for embarrassment here: the sight of your beloved child is guaranteed to trigger the release of oxytocin.
In order not to experience discomfort, you need to take a comfortable position. You can turn off the lights and sit in a soft chair, turn on pleasant music. From a medical point of view, the best position for pumping is sitting, slightly leaning forward.
How to properly express breast milk
Having prepared the containers and breasts, you can start pumping. Before starting, you need to wash your hands with soap.
- Place one hand under the breast to support the mammary gland.
- Place your other hand on your chest - your thumb above the nipple, slightly above the areola. Index - under the areola. Your fingers should form a C shape around the areola of the nipple.
- Squeeze your index finger and thumb lightly, as if directing the flow of milk outward. Movements should be rhythmic and smooth. Pumping shouldn't be painful.
- The lower hand can be released and used to hold the milk container.
- As soon as the flow of milk has decreased, you need to slightly change the place of pressure (thumb position). Thus, you need to go through the entire gland in a circle.
- If lactation has already been established, there is no point in expressing until the last drop, because it simply won’t be there. Valuable liquid will be formed directly during the pumping process. You need to stop when the flow of milk has weakened significantly, or the planned volume of milk has been reached.
 The position of the fingers near the areola needs to be changed to free all the ducts
The position of the fingers near the areola needs to be changed to free all the ducts When using a breast pump, you need to do all the preparation and then follow the instructions of the device. A comfortable position and complete relaxation will help you survive pumping without damaging your nipples or causing nervous tension.
When expressing, there is no point in putting pressure on the nipple - this can only injure it. It is necessary to influence the mammary gland itself.
How often should you pump?
There is no general rule regarding the number of pumping sessions per day. Everything is determined in a specific situation. Only some general recommendations can be described:
- If the baby is full term, born healthy, quickly latched onto the breast and suckles well, there is no need to express. Attaching a baby on demand will be the best prevention of congestion.
- If the baby does not immediately take the breast in the first days, he is lethargic and sleepy for some reason, then he will need to be woken up for feedings. If, upon waking up, the baby actively sucks for less than 10 minutes, you will have to pump the milk for the same amount of time. It is advisable to give everything that has been expressed to the child from a syringe or pipette. This will need to be done every couple of hours. Upon discharge, the pediatrician will give his recommendations.
- If the baby was born too early and was admitted to intensive care, the mother will need to pump every 2-3 hours for 15 minutes, regardless of the amount of milk. This will allow you to maintain lactation by the time the baby is discharged.
- If the breast is literally swollen from too much milk, the breast will need to be emptied slightly before feeding to make it easier for the baby to latch on to the nipple. If stagnation and overcrowding bother you greatly, you can express completely once a day. If lactostasis begins (thickness appears and the temperature rises) - 2-3 times a day, but not more often! The more often a woman expresses, the more milk will come - it will be a vicious circle. It is best to do this little by little until the discomfort goes away.
- If for some reason the mother is not near the baby, but wants to support lactation, she will need to express 7–8 times a day, of which at least once at night.
The amount of milk that can be expressed at one time varies from woman to woman. It depends on the stage of lactation, time of day and many other factors that influence lactation “here and now.” The average portion of milk for women with established lactation is 130 ml at a time, but you should not rely on this figure. Whether there is enough milk is determined by the baby’s weight.
Doing the procedure for the first time
For those who do not have experience pumping, it is best to do it under the supervision of a specialist. In maternity hospitals, midwives or nurses are required to help women in this matter. They will show you how to work with your hands and what is the best position to take.
The first pumping should be done manually. This will be the gentlest way for the still tender breasts. With this approach, it will be easier to understand your sensations and see exactly what movements help push milk out of the ducts. It will be possible to “find” the appropriate speed and intensity of movements. If a woman plans to use a breast pump in the future, you should not set the device to high intensity the first time.
Before pumping for the first time, it is advisable to watch the video instructions. This will help you make sure your actions are correct.
Breast preparation and pumping - video from the Union of Pediatricians of Russia
Storage and use
Expressed milk can be used immediately, stored in the refrigerator or frozen.
If for some reason a woman cannot feed the baby directly from the breast (for example, a painful crack), she can express milk and give it to the baby in a bottle. Freshly expressed milk does not need to be heated in the summer, but if the apartment is cool and it has cooled down greatly during the pumping process, you can slightly warm it up.
There are two ways to heat breast milk - in a special warmer or in a water bath (when a bottle of milk is placed in a jar or saucepan with warm water).
Do not use a microwave to heat breast milk! Microwave waves destroy the beneficial properties of this valuable liquid. In addition, you can easily overheat the milk.
For those who like to express for future use (for the next few days or just “in reserve”), a refrigerator or freezer will help preserve milk. If you are unable to collect enough milk in one pumping session, you can mix portions from different pumping sessions. But this should only be done with a chilled product! That is, both portions should stand in the refrigerator for some time, and only after that they can be poured into one storage container.
The shelf life of milk for healthy children and babies being cared for in a maternity hospital is different.
Table: product shelf life
To defrost breast milk, it is advisable to put it out of the freezer and into the refrigerator in advance. If you need to feed your baby urgently, you can defrost the milk at room temperature. Breast milk thaws very quickly, so there is no need to warm it up with anything.  The supply of milk in the freezer is called a “bank”: the date of pumping must be written on each container
The supply of milk in the freezer is called a “bank”: the date of pumping must be written on each container
There is probably not a single moment in breastfeeding on which every mother would not have her own opinion. Take pumping, for example. Some women, relying on the experience of previous generations, believe that breast milk must be expressed after each feeding; others argue that this can only be done under certain circumstances. Who is right?
What happened before
Previously, a nursing mother was recommended to express her breasts after each feeding, otherwise there would be excess milk, lactostasis and mastitis, and in addition, it was believed that pumping promoted milk production and the baby would certainly not remain hungry. Yes, pumping increased the amount of milk, but this did not take into account the fact that the mother’s breast adapts to the baby’s needs - and produces exactly as much milk as the baby sucks. It is now known that if after each feeding the breast is additionally expressed, then the breastfeeding woman’s body receives incorrect information about how much milk needs to be produced, and produces more and more of it. As a result, expressing the “leftovers” can turn into a continuous process: with each expression the milk comes in, the baby cannot suck it completely, the mother must express the leftovers, and by the next feeding the milk again comes in excess.
What's wrong with that? Excess milk is a direct road to stagnation (lactostasis), and a woman is forced to constantly express her breasts. It turns out to be a kind of vicious circle.
What are they saying now?
Today, doctors recommend feeding a newborn on demand; with this regimen, he eats the amount of milk that he needs. By the next feeding, the required amount comes again, and no pumping is necessary. Yes, there will be periods of baby's growth when he will need more milk than before, but the baby will regulate this process himself. At some point, the baby will begin to suckle more intensely and ask for the breast more often than before. At first it will seem to the mother that there is not enough milk, but in a couple of days everything will stabilize, milk will begin to come in the required (larger) quantity and no pumping, much less additional feeding, will be required.
When is pumping necessary?
It turns out that pumping is not necessary at all? Most often, yes, but there are still some situations when you simply cannot do without it.
When is pumping necessary:
1. If the baby is premature or weak, he cannot yet suckle on his own and must be bottle-fed.
2. If the mother has a very strong milk flow, incipient mastitis or the first signs of lactostasis. In general, with a strong flow of milk and lactostasis, it is recommended to put the baby to the breast more often, but if he is not hungry, then the breast will have to be expressed.
3. If there is not enough milk, but only if it is, and not “it seems so to me” or “my mother-in-law said that I don’t have enough milk and need to express myself.”
4. If you need to part with your baby for a while, but at the same time you want to maintain lactation.
5. If a nursing mother gets sick and is prescribed medications that are incompatible with breastfeeding.
How it works
If you still need to express your breasts, you can do this with your hands or using a breast pump. The advantage of manual expression is that there are no material costs, but, perhaps, this is all its advantages. There are many more disadvantages: not all mothers know how to express their breasts correctly (even after looking at the instructions). And most importantly, manual expression is not as effective as mechanical expression, and in general is often unpleasant and even painful. But expressing your breasts with a breast pump is much more convenient: it quickly helps you express a significant amount of milk, saves time and effort and does not cause pain. And there is only one minus - it costs money.
How to choose a breast pump
- Do not rely on the opinions of friends and reviews on the Internet: like someone else’s breasts, it is impossible to try on someone else’s experience of pumping.
- Carefully examine the breast pump model. A device that has already been purchased or given as a gift may not be suitable for the size of the funnel, the intensity of pumping, the shape of the handle, the number of parts, or the noise level.
- The more often you plan to express, the more advanced and versatile breast pump you need.
- Strictly follow the instructions supplied with the device. Remember to sterilize your breast pump before each use and keep it clean.
- Don’t get carried away: if you use it too intensively, there is a risk of hyperlactation - more and more milk will be produced, and as a result, pumping will be endless.
Why problems arise
Sometimes mothers say that a breast pump, of course, helps, but they would like it to be used. O greater effect. There may be several explanations for this. Or there is really little milk, and then you need to express at least a couple more minutes after the last drop appears. Or the device itself turned out to be not very suitable for a particular breast .
For example, manual breast pumps are much less convenient and efficient than electric ones. They essentially imitate manual expression, just a little more comfortable. But their price is low.
So if you really need a breast pump, then it is better to choose models with high power, pumping both breasts at the same time, electric, stationary, with the ability to change traction and speed. There are no problems at all with such breast pumps: put it on your breast, turn on the button - and go about your business.
As you can see, there is no clear opinion about pumping. With normal, well-established lactation it is not necessary, but it becomes necessary in case of some problems. The same can be said about a breast pump. And if so, then we feed calmly, focusing only on our situation and the needs of our baby.