Hygiene education plays an important role in the formation of a high sanitary culture of the population and health literacy. Children from an early age need to be explained the meaning and significance of each hygiene skill. Considering that skills are a kind of reflexes, they must be performed systematically, sequentially, at the same time.
Parents, medical workers, educators, teachers, educators, as well as the media should instill hygiene skills in children. Middle and high school students have long been familiar with basic hygiene rules, but do not always follow them.
INTRODUCTION
The air always contains one or another number of microorganisms. They spread with the help of air. Pathogenic microbes can spread through the air, causing plant diseases, animals and humans.
The number of microorganisms in 1 cubic meter of air in different places can reach the following sizes: in a barnyard up to 2 million; in residential premises - 20 thousand; on city streets - 5 thousand; in parks - 200; in sea air - 1-2.
Target
a clear justification for the need to comply with school hygiene rules.
Tasks
1. Test the air in the gymnasium classrooms for microbial contamination (before, after classes and after an hour of ventilation) using the sedimentation method.
2. Examine the microflora of the skin of schoolchildren’s hands (immediately after a physical education lesson, after treating with a damp cloth and washing hands with soap).
3. Promote hygiene practices during training sessions.
STUDY
Microflora of indoor air more uniform and relatively stable. Among microorganisms, the inhabitants of the human nasopharynx dominate, including pathogenic species that enter the air when coughing, sneezing or talking. The main source of air pollution by pathogenic species is bacteria carriers. The level of microbial contamination depends mainly on the population density, human traffic, the sanitary condition of the premises, including dust pollution, ventilation, frequency of ventilation, cleaning method, degree of illumination and other conditions. Thus, regular ventilation and wet cleaning of premises reduces air contamination by 30 times (compared to control rooms). Self-cleaning of indoor air does not occur.
In countries with cold climates, it is natural to want to save energy by reducing ventilation when cold weather sets in, just to maintain indoor air quality at a minimum acceptable level. Over the past 20 years, allergic reactions and cases of asthma have become twice as common in the economically developed countries of the world. This disease is becoming one of the most important health problems. Huge amounts of money are required for medicines, patient care and compensation for temporary disability. It has been hypothesized that the main cause of this problem is the deterioration of indoor air quality. Rising energy tariffs and, in particular, electricity tariffs, large-scale campaigns to stimulate energy saving lead to insulation and “sealing” of homes while simultaneously reducing ventilation costs.
Studies conducted in Denmark and Sweden have shown a clear correlation between the productivity of typical office work and air quality. The same problem exists in schools, where air quality is often not very good.
Microflora of indoor air
Air is an environment in which microorganisms are not able to reproduce, due to the lack of nutrients and lack of moisture. The viability of microorganisms in the air is ensured by suspended particles of water, mucus, dust, pieces of soil, etc. Atmospheric air and indoor air differ significantly in the quantitative and qualitative composition of microflora. Bacterial contamination of residential premises sometimes exceeds the contamination of atmospheric air, including pathogenic microorganisms entering the air from sick people, animals and bacteria carriers. Air microflora is conventionally divided into resident (more often detected) and temporary (detected occasionally).
The permanent air microflora is formed by soil organisms; it relatively regularly includes Micrococcus roseus, M. flavus, M. candicans, Sarcina flava, S. Alba, S. Rosea, Bacillus subtilis, B. Mycoides, B. Mesentericus, all species Actinomyces, Penicillium, Aspergillus, Mucor, etc.
Temporary air microflora is also formed mainly due to soil microorganisms, as well as due to species coming from the surface of water bodies.
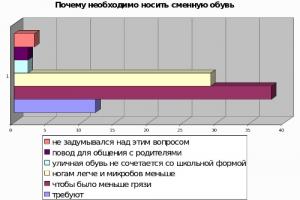
The microflora of the air is very dynamic and undergoes continuous renewal. The saturation of the air in gymnasium classrooms with microorganisms occurs mainly by droplets in the aerosol formed when talking, coughing, sneezing, and also introduced with dirty shoes. A survey about the need to wear replacement shoes showed that, for the most part, students know why it is necessary to change shoes in the gymnasium.

With the onset of the slushy season, the problem of wet feet becomes relevant for almost every teacher, parent and student. Autumn and winter shoes take a very long time to dry naturally, and wearing wet shoes leads not only to hypothermia and colds, but also to the development of fungal microorganisms. A humid and warm environment is ideal for fungus, which affects the skin of the feet and leads to unaesthetic and dangerous changes in the appearance of the foot and the appearance of an unpleasant odor. A strong argument in favor of wearing a “change.”
Methodology for conducting an experiment to identify the general microbial contamination of air
Material for research: indoor air.
Method: sedimentation.
Result: information is provided about the absence or presence of pathogenic microorganisms in the air.
The sedimentation method (cup method) is the simplest method for studying air microflora, although it does not have great accuracy. If cups of the same diameter are used for the same exposure period, then this method can be used to obtain comparative data on bacterial air pollution. The technique of this method is as follows. Petri dishes with frozen agar are exposed open at different heights in the room for different periods of time (from 15 minutes to 1.5 hours). Then the cups are closed and placed in a thermostat. The crops are incubated for 24 hours. Over the course of a day in a thermostat, each bacterium produces a whole colony; counting colonies allows one to assess microbial air pollution.
To recalculate the number of microbes per 1 m3, they use Omelyansky’s formula, who believed that during a 10-minute exposure, as many microbes settle on the surface of a dense nutrient medium of 100 cm2 as there are in 10 liters of air (1:100 m3). He compiled a corresponding calculation table, using which you can calculate the total number of microorganisms in 1 m 3 of air.
Calculation of the number of microbes in 1 m 3 of air according to Omelyansky.
Calculation of microbial content in 1 m 3 of air in gymnasium classrooms

For greater clarity, on the same day, samples were taken from the classroom before classes (after a day off), after the first lesson, after the second lesson, after the sixth lesson, after cleaning and airing.





Microflora of human skin
The skin is ubiquitously and quite abundantly populated by bacteria and fungi. The permanent inhabitants of the skin are aerobic and anaerobic, lipophilic and non-lipophilic bacteria and yeast-like fungi, fecal streptococci, E. coli and many others. The composition of the skin microflora depends on age, degree of hair growth, humidity, temperature, acidity, profession, hygienic maintenance of the skin, skin and general diseases (diabetes, jaundice, uremia, leukemia). A significant impact on the composition of the skin microflora is exerted by hospital stays (colonization with hospital variants of bacteria), prolonged use of antiseptics, and corticosteroids.
The skin is unevenly populated with microbes. There are many of them on the surface and under the first and second layers of keratinized epithelium. There are also a lot of microbes in the mouths of hair follicles. Microbes are found in hair follicles. The sweat and sebaceous glands are usually free of microbes due to the antibacterial activity of fatty acids and lactic acid. The distribution of microbes on the skin surface is also heterogeneous. Wet and hairy areas are abundantly populated (perineum, inguinal folds, axillary fossae, interdigital spaces of the feet, terminal phalanges of the hands). An increased number of microbes is found in sebaceous areas (face, chest, back, hair).
The normal microflora of the skin performs a protective function, inhibiting the vital activity of foreign pathogenic and opportunistic microbes. At the same time, the skin can serve as a source of exogenous infection and autoinfection (diseases caused by its own opportunistic microbial flora, which acquires pathogenic properties under unfavorable conditions for the body). Particularly dangerous in this regard is the microflora of the hands and perineum, often containing staphylococci and enterobacteria (a large family of bacteria that includes such well-known pathogens as: salmonella, E. coli, plague bacillus). On the feet and between the toes there are often large quantities of fungi that cause dermatomycosis, which are transmitted to other people with shoes. The accumulation of germs in damp areas can cause foul odors.
Microbiologists from the National Institutes of Health in the USA conducted a census of the types of bacteria living on the surface of human skin. Their research made it possible for the first time to draw up a detailed map showing the prevalence of microorganisms on the human body.
The report of American scientists was published in the journal Science. In the study, they scraped flakes of skin from 20 different areas of the body of 10 people. Before this, the experiment participants were asked to wash with regular (not antibacterial) soap for a week - to get a picture typical of the average healthy person. Such tests have been done by doctors before, but the researchers went further, using a method of analyzing the genetic material of the bacteria they collected.
The method of analyzing the so-called ribosomal RNA made it possible to determine which groups of bacteria the scientists encountered. In addition, in this way it was possible to find representatives of 19 different types of bacteria.
The term “phylum” in biological taxonomy corresponds to a very large group that unites a wide variety of organisms. Humans and flounder belong to the same phylum, and the discovery of 19 types of bacteria out of 27 existing ones indicates a high diversity of skin microflora. For convenience, scientists have proposed dividing skin areas into three types: wet, oily and dry. In oily areas of the skin (eyebrows, wings of the nose), biologists found the least number of different types of bacteria: despite the fact that it is in such areas that microorganisms that cause the development of acne live.
Wet areas of the skin are the nasal cavity, the area between the fingers and the armpits. It is humid areas that are an ideal ecosystem for the development of all types of bacteria; in terms of diversity and population, researchers compared such areas with tropical forests.
In dry areas of the skin (the upper side of the palm and buttocks), according to scientists, bacteria do not really “like” living: the researchers found the skin behind the ears to be the most unsuitable area for microbes to live. It must be remembered that the older the child gets, the more bacteria begins to develop on his skin.
Methodology for conducting an experiment to identify microorganisms on the surface of the skin
The material for research is the skin of the hands.
Equipment and materials: containers with a dense nutrient medium.
Result: information about the number of bacteria on the fingers.
Sowing is done in 3 Petri dishes as follows: the lid of the dish is slightly opened and light imprints are made on the surface of the medium with the pad of your finger after exercising in the gym, after treating your hands with a damp cloth, after washing your hands with soap. Touch the medium carefully so as not to push it through.
After 2–5 days, we inspect the containers and compare the number and variety of microbial colonies that have grown from fingerprints.
A fingerprint has an area of about 1 cm2. The area of the palm is about 150 cm2 (our own calculations). Knowing the number of germinated colonies, we can guess how many microbes there may be on one student’s hand.

CONCLUSION
The goal of the work has been achieved - microbiological experiments clearly demonstrate the need to comply with such hygienic rules as wearing replaceable shoes, the need for high-quality wet cleaning and regular ventilation, washing hands during the school day after physical education lessons, after visiting the toilet, before eating. The results of the study are brought to the attention of gymnasium students, posted on the gymnasium website, and can also be used by class teachers to conduct thematic classes.
Supervisor
Topchieva Irina Vladimirovna
biology teacher of the highest qualification category
Leningradsky district
Municipal educational institution, gymnasium of the village of Leningradskaya
The surface of human skin, especially its exposed parts, is contaminated with various microorganisms; here, from 25,000,000 to 1,000,000,000 microbial individuals are determined.
The native microflora of human skin is represented by sarcins, staphylococci, diphtheroids, some types of streptococci, bacilli, fungi, etc.
In addition to the microflora characteristic of the skin, transient microorganisms may be present here, which quickly disappear under the influence of the bactericidal properties of the skin. Cleanly washed skin has a great ability to self-cleanse. The bactericidal nature of the skin reflects the general resistance of the body.
Intact skin is impenetrable to most microorganisms, including pathogenic ones. If their integrity is violated and the body's resistance decreases, skin diseases can occur.
Sanitary and bacteriological examination of the skin
Sanitary and bacteriological examination of the skin is carried out using two methods:
Sowing fingerprints on MPA in Petri dishes, followed by macroscopic and microscopic examination of the grown colonies.
Culture of skin swabs to determine the total microbial count and E. coli.
Using a swab soaked in 10 ml of sterile saline, carefully wipe the palms, subungual, and interdigital spaces of both hands. The tampon is rinsed in a test tube with saline solution and the initial wash is examined for the total microbial count and the presence of E. coli.
Determination of total microbial count
1 ml of the wash is placed in a sterile Petri dish, 12-15 ml of melted and cooled to 45 0 MPa is poured, the contents of the dish are mixed and after the agar has solidified, the crops are incubated at 37 0 C for 24-48 hours. The grown colonies on the surface and in the depth of the agar can be counted done using a magnifying glass.
Definition of Escherichia coli
The remaining amount of the wash is placed in a test tube with glucose-peptone medium. The crops are incubated at 43 0 C for 24 hours. If gas formation occurs, they are sown on Endo medium. The growth of red colonies on this medium will indicate the presence of E. coli in the washout, indicating fecal contamination of the hands.
Microflora of the oral cavity
The oral cavity has favorable conditions for the development of microorganisms: the presence of nutrients, optimal temperature, humidity, and the alkaline reaction of saliva.
In maintaining the qualitative and quantitative constancy of the normal microflora of the oral cavity, the main role is played by saliva, which has antibacterial activity due to the enzymes it contains (lysozyme, lactoferrin, peroxidase, nuclease) and secretory immunoglobulins.
By the end of the first week, streptococci, Neisseria, lactobacilli, yeast-like fungi, and actinomycetes are found in the oral cavity of newborns. The quantitative and species composition of oral microbes depends on the diet and age of the child. During teething, obligate gram-negative anaerobes appear.
More than 100 species of microorganisms are found in the oral cavity, most of which are aerobes and facultative anaerobes.
The bulk of oral microorganisms are localized in dental plaque: 1 mg of dry mass of dental plaque contains about 250 million microbial cells. A large number of microorganisms are found at the neck of the tooth, in the space between the teeth and in other parts of the oral cavity that are inaccessible to washing with saliva, as well as on the mucous membranes of the pharyngeal tonsils. Individual fluctuations in the qualitative and quantitative composition of the oral microflora depend on age, diet, hygiene skills, resistance of the mucous membrane, and the presence of pathological processes in the teeth and gums.
The resident group of oral bacteria consists of streptococci (Streptococcussalivarius), non-pathogenic staphylococci, saprophytic neisseria, corynobacteria, lactobacilli, bacteroides, fusiform bacteria, yeast-like fungi, actinomycetes, mycoplasmas (M.orule), protozoa (Entamoebabuccalis).
Among the facultative microorganisms there are enterobacteria (genus Esherichia, Klebsiella, Enterobacter, Proteus), Pseudomonas aeruginosa, spore-forming bacteria (genus Bacillus, Clostridium), microorganisms of the genus Campylobacter (C.consicus, C.sputorum).
For qualitative and quantitative study of the microflora of the oral cavity, bacterioscopic and bacteriological research methods are used.
Bacterioscopic method. The material being studied is dental plaque. The smear is stained with Gram or Burri and the morphological and tinctorial properties of microorganisms are studied.
Bacteriological method. The material for the study is mucus from the throat, which is collected using a sterile cotton swab. Inoculate with the same swab in streaks onto a Petri dish with blood agar. After daily incubation at 37 0 C, smears are prepared from the grown colonies, stained with Gram, and the morphological and tinctorial properties of the isolated culture of microorganisms are studied.
Due to constant contact with the external environment, the skin most often becomes a habitat for transient microorganisms. However, there is a stable and well-studied permanent microflora, the composition of which varies in different anatomical zones depending on the oxygen content in the environment surrounding the bacteria (aerobes – anaerobes) and proximity to mucous membranes (mouth, nose, perianal area), secretion characteristics, and even human clothing.
Particularly abundantly populated by microorganisms are those areas of the skin that are protected from light and drying: armpits, interdigital spaces, inguinal folds, perineum. At the same time, microorganisms of the skin are affected by bactericidal factors of the sebaceous and sweat glands.
The first microbes enter human skin during the passage of the mother’s birth canal, and then from the air of the maternity hospital, from the hands of staff and from the skin of the mother’s mammary gland. During this period, staphylococci and fungi of the genus Candida, which are later replaced by normal microflora.
The resident microflora of the skin and mucous membranes includes: S. epidermidis; Micrococcus spp.; Sarcina spp.; coryneform bacteria ; Propionibacterium spp.
As part of the transitory: S. аureus, Streptococcus spp., Peptococcus spp., Bacillus subtilis, Escherichia coli, Enterobacter spp., Acinetobacter spp., Lactobacillus spp., Candida albicans and many others.
In areas where there are accumulations of sebaceous glands (genitals, outer ear), acid-fast non-pathogenic mycobacteria are found. The most stable and at the same time very convenient for study is the microflora of the forehead area.
The vast majority of microorganisms, including pathogenic ones, do not penetrate intact skin and die under the influence of the bactericidal properties of the skin.
Factors that can have a significant impact on the removal of non-persistent microorganisms from the skin surface include: acidic reaction of the environment, the presence of fatty acids in the secretions of the sebaceous glands and the presence of lysozyme.
Neither excessive sweating, nor washing or bathing can remove the normal permanent microflora or significantly affect its composition, because the microflora is quickly restored due to the release of microorganisms from the sebaceous and sweat glands, even in cases where contact with other areas of the skin or with the external environment is completely stopped. Therefore, an increase in the contamination of a particular area of the skin as a result of a decrease in the bactericidal properties of the skin can serve as an indicator of a decrease in the immunological reactivity of the macroorganism.
The causative agents of purulent-inflammatory processes can be representatives of various genera, the vast majority of which are classified as so-called “opportunistic” microflora (aerobic, microaerophilic, facultative anaerobic and anaerobic). Among them, the most common types of childbirth are: Staphylococcus, Streptococcus, Pseudomonas, Escherichia, Proteus, Citrobacter, Klebsiella, Enterobacter, Hafnia, Serratia, Aeromonas, Alcaligenes, Acinetobacter, Haemophilus, Peptococcus, Bacillus, Clostridium, Corynebacterium, Propionibacterium, Bacteroides, Nocardia, Listeria, Fusobacterium, Neisseria, Mycrococ cus, Mycoplasma. Less often - Yersinia, Ervinia, Salmonella, Acinetobacter, Moraxella, Brucella, Candida, Actinomyces.
Microorganisms can cause and maintain a purulent process, both in monoculture and in association.
The human microflora is a collection of many microbiocenoses, includes hundreds of different species and is almost an order of magnitude larger in number than the number of cells of all organs and tissues of the human body.
All open cavities and human skin are populated by microbial populations that are most adapted to the specific conditions of each specific biotope. Microbiocenoses arose in places of contact of the human body with the environment - skin, gastrointestinal mucosa, vagina. They are in a state of dynamic equilibrium with changing environmental conditions.
The physiological status of the body and the state of its nonspecific protective forces are associated with the vital activity of microflora. Representatives of normal microflora protect the skin and mucous membranes from penetration and rapid reproduction of pathogenic and opportunistic microorganisms, and perform a number of other functions.
Microbiocenoses of the human body are unique endogenous microbial genetic funds. They store a huge amount of genetic information, both plasmid and chromosomal. Obligate microflora adhered to the epithelium is capable of exchanging genetic information with the cells of the macroorganism. The human genome contains nucleotide sequences characteristic of more than 200 species of bacteria and 500 species of retroviruses. Through endocytosis, the microflora can receive cellular material from the host and transfer its antigens to the cells of the macroorganism. Thus, the microflora acquires receptors or host antigens and, accordingly, protection from the immune system. This may also explain the widespread distribution of cross-reacting antigens of certain microbial cells and tissues of the host body. This group of antigens is one of the factors inducing the development of autoimmune conditions.
The composition and functions of human microbial biocenoses depend on:
· age,
· nutritional characteristics,
· climate,
· environmental conditions, etc.
A healthy lifestyle and lack of stress support non-pathogenic biocenoses. Age-related changes can contribute to a decrease or increase in the pathogenicity of a number of pathogens.
The influence of environmental factors modifies not only the protective forces of the macroorganism, but also changes the properties of the microorganism.
Microbial biocenoses are quite sensitive biological systems that respond to many factors. For example, with inadequate or reduced nutrition, the dynamics of changes in microbiocenoses in various biotopes of the human body is of the same type - there is a decrease in the number of resident forms of bacteria with an increase in the number of opportunistic and pathogenic species.
Changes in the species composition of microbiocenoses of the body of a healthy person and its immunobiological factors reflect the stage of tension of adaptation mechanisms.
To assess the homeostasis of the body and monitor the nutritional status of people, we can recommend the study of microbiocenoses of the skin and pharynx, as they are the most accessible and quickly respond to external influences.
Individual microbial biocenoses actively interact with each other and with the host organism. The total number of microbial cells colonizing the human body is 1–3 orders of magnitude greater than all the cells that make up all human organs. The most densely populated ecosystem is colonic biotope(about 60% of human microflora is concentrated in it). 15–20% of microbial populations inhabit skin. 15–16% of microorganisms are in oropharynx, V vaginal biotope Women contain 9–10% microflora.
Given the multicomponent nature of the human microflora, the basis of normal microbiocenoses of all open cavities and skin is made up of only a few groups of indigenous bacteria, among which saccharolytic, asporogenic, non-pathogenic anaerobes always dominate. These include bifidobacteria, lactobacilli and propionic acid bacteria, which represent the basic component main (obligate, indigenous, resident) human microflora.
Thus, lactobacilli are found in all biotopes of the digestive tract, starting from the oral cavity and ending with the rectum, and are the dominant flora of the vaginal biotope.
Different biotopes are characterized by certain species specificity: epidermal staphylococci predominate in the deep microflora of the skin, non-pathogenic streptococci predominate in the microflora of the nasopharynx, and bifidobacteria and lactobacilli occupy a dominant position in the intestinal microbiocenosis.
Bacteria of the genus Staphylococcus are in most cases sown from all biotopes of the human body. Normally, they are represented by saprophytic staphylococci, mainly from the species S. epidermidis.. Pathogenic staphylococci (S. aureus) are found in small quantities and, with normal functioning of the microecological system, do not cause pathological processes in the body. The development of endogenous staphylococcal infections is possible only with a decrease in the colonization resistance of the body.
In a healthy human body, the microbiocenosis, consisting of a high population level of indigenous protective flora and a small number of opportunistic microorganisms, is an open self-regulating ecosystem. This ecosystem is capable of independently maintaining an optimal ratio between individual groups of microbiota. The constant presence of opportunistic microorganisms in the biocenosis makes a certain contribution to the positive effect of eubiosis on the host organism. Their permissible concentration is strictly controlled by the protective properties of the indigenous normal flora and the host’s immune system. Opportunistic microorganisms participate in the biosynthetic, metabolic and digestive functions of the microbiocenosis, and constant antigenic irritation of the intestinal wall stimulates the local immune mechanisms of the macroorganism.
If the optimal relationship between the components of the biocenosis is violated, some of its normal representatives can cause endogenous infections. Dysbiosis leads to sensitization of the body with many clinical manifestations of allergies, can cause intoxication, exhibit mutagenic properties and have many other negative effects on the body.
All local microecosystems closely interact with each other and with the host organism, forming a single symbiotic system due to the presence of complex and diverse regulatory mechanisms. In this case, a single microecological system (microbiota) is formed, which is an important multifunctional integral part of the human body.
Thanks to the “cooperation” between the organisms inhabiting the macroorganism, the human microecological system acts as a single whole, working in concert for the system in which it is localized. The mechanisms for maintaining the stability of qualitative and quantitative parameters of human microflora have not been fully studied.
The symbiotic relationship between the host organism and its autoflora suggests the presence of a complex and multifaceted mechanism. This mechanism is implemented at the metabolic, regulatory, intracellular and molecular genetic levels. These relationships are vital for both humans and the microbial populations inhabiting their bodies.
Therefore, isolating one pathogen as the leading etiological factor is not always possible. In the vast majority of cases, we should be talking about a pathogenic biocenosis or microbial biofilm.
The microbiocenosis of various human organs and cavities is a very sensitive indicator system. This system is capable of responding with qualitative and quantitative changes to any physiological and pathological changes in the state of the macroorganism and preventing the invasion of pathogenic microorganisms.
Assessment of the qualitative and quantitative composition of resident microflora and identification of indicator microorganisms make it possible to assess the stage of adaptation, as well as make a pre-nosological diagnosis of the status of the body, reflecting the functional state of the barrier-protective functions of the skin, the local humoral system of the gastrointestinal tract (saliva) and excretory subsystems (urine). With the development of adaptation, the number of indicator microorganisms and their associations changes (sowing representatives of 2-3 genera of 1 family at the same time). A system for assessing an organism based on microecological indicators can be used as an indicator of the adverse effects of chemical pollution of the environment.
In various biological environments there is “ critical microbial number»
· Borderline states of the body: in saliva - up to 50 colonies, microbial associations - up to 10 colonies; on the skin – up to 30 and up to 5, respectively; in urine - up to 50 and up to 10, respectively),
· Failure of adaptation: saliva - over 50 and 10, respectively, etc.,
Pathological disorders in the body: in saliva above 100 and 60, respectively, on the skin - over 80 and 40, in urine - over 200 and 70.
In the last decades of the 20th century there was a radical change in the microenvironment in the human community. Under the influence of environmental pollution and antibacterial agents, the stable human bacterial microbiocenosis was destroyed. Biologically viable symbioses with bacteria have been lost. The endoecological balance is disrupted in favor of the viral microenvironment.
As a result, slow viral infections, including AIDS, can be considered as a symptom of deep genetic disorders of the internal environment of the human body caused by a change in microbiocenosis.
The biological state of the human body has changed. There has been a transition from bacterial carriage and symbiosis with the bacterial internal environment, functioning on the principles of mutualism - the highest form of mutually beneficial symbiont relationships, to a new state. This condition creates favorable conditions for long-term persistence of viruses in the human body.
Dysbacteriosis- changes in the composition and quantitative ratios of microflora that normally populate hollow organs communicating with the environment (upper respiratory tract, intestines) and human skin.
Formation of human microflora.
As is known, the gastrointestinal tract of a newborn is sterile. Within a few hours after birth, it begins to be colonized by strains of bifidobacteria. streptococci, Escherichia coli, etc. After a day, anaerobic lactobacilli and enterococci can already be detected in the intestines, and from about the 10th day, bacteroids multiply intensively. After about a month, a stable and at the same time individual microbiocenosis is established.
The colonization of the human body by microflora begins during the passage of the fetus through the mother’s genital tract during childbirth. Therefore, the main source of the initial microorganisms on the basis of which the biocenoses of each individual are formed are representatives of the mother’s vaginal biocenosis.
The main microorganism that determines intestinal biocinosis is bacteria bifidum. To colonize bifidobacteria, β-lactase from human milk is required (cow's milk contains α-lactase).
The formation of the microflora of a newborn baby is determined:
1. The state of the microflora of the mother’s intestines and vagina;
2. The state of the microflora of the maternity room;
3. The state of the microflora of the skin and breast nipples;
4. Type of feeding (artificial feeding contributes to the development of dysbiosis);
5. Taking medications and, above all, antibiotics;
6. Injected preparations of pure cultures of microorganisms.
Formation of qualitative and quantitative composition of microflora:
· regulated by the mechanism of intermicrobial interactions within each microecosystem,
· controlled by physiological factors of the host’s body in the dynamics of its life.
The activity of microorganisms depends on the factors of the internal environment of the body:
· biochemical (level of cholesterol, peroxides, superoxide radicals, hormones, etc.)
· biophysical (pH, temperature, osmotic pressure, etc.) indicators.
There is a complex spatiotemporal picture of changes in microbiocenoses in the human body. Pathogenic microorganisms can appear, disappear and reappear in different parts of the body. This is due to both the microbes’ own activity and changes in local immunity, capillary blood flow, lymphodynamics, local releases of hormones, etc.
In orthodox medicine there are no methods and means of monitoring and predicting such a spatio-temporal picture. For example, in a patient, laboratory diagnostics of materials from the urogenital tract do not reveal the actor Ureaoplasma urealyticum. At the same time, they cause an active inflammatory process in the joints and, upon more detailed examination, are detected in the synovial fluid.
Microbiocenosis of the skin.
The skin is considered the largest organ of the human body. It represents a unique system closely related to the internal environment of the body and its external environment.
The skin is abundantly populated by microorganisms. Microbial contamination, depending on the area of the skin, varies from several units to hundreds of thousands of cells per square centimeter. The indigenous flora is concentrated in the deeper layers, in the area of the mouths of the pilosebaceous follicles. The surface microflora of the skin is usually random.
Skin microbiocenosis has been little studied. There is evidence that the most common representatives of skin microflora are staphylococci (S. epidermidis and S. saprofiticus) and fungi of the genus Candida.
Normal skin microflora plays an important role in maintaining body homeostasis. The microflora of the skin is closely connected with the state of the macroorganism, with its immune status. Adverse effects on the body, causing immune suppression, are accompanied by characteristic changes in the microecology of the skin with the development of dysbacteriosis.
Characteristics of skin microbiocenosis is a very sensitive indicator of the immunoreactive state of the human body. Under the influence of unfavorable factors, a structural restructuring of the skin microbiocenosis occurs, accompanied by a change in absolute dominants and an increase in species diversity. These changes are directly dependent on the duration of the adverse effect.
When exposed to harmful environmental factors, the number of normal symbionts decreases and opportunistic microorganisms grow. With a decrease in the resistance of the human body, opportunistic microorganisms are able to exhibit their pathogenicity.
Skin is the protective barrier of the human body. She is sensitive to the sun's rays, wind, and season changes. Poor lifestyle and diet lead to rashes and redness. You need to take good care of your skin, but first you need to become familiar with its structure and microflora. This is important in order to better know how to treat skin problems and... This article will tell you everything about the structure of the skin and the microorganisms that live in it.
Skin structure and function
The skin is not a simple organ, as it seems at first glance. It performs special functions in the human body and has a complex structure. It reflects all internal diseases of the body. And the skin itself protects against dirt and the penetration of pathogenic bacteria. The structure of the skin includes:
- sweat and sebaceous glands,
- sebum,
- hair follicles,
- nails.
The structure of the skin is as follows:
- The epidermis, which is divided, in turn, into five layers of cells.
- Dermis. The actual skin, which contains hair follicles, glands, nerve endings, blood vessels, and so on.
- Hypodermis or subcutaneous fat layer.
The functions of the skin include:
- protection;
- excretion of metabolic products;
- water-salt metabolism;
- thermoregulation;
- breath;
- tactile function.
As can be seen from the above, the skin performs vital functions. Injuries and diseases of the skin should not be underestimated. You should be careful about their health. After all, this is the beauty and youth of a person, his serious protection from the external unfavorable environment.
Other symptoms, such as dryness, sagging, and dull complexion, can also be treated using their own methods. For each skin type, medications are selected; if necessary, injections can be prescribed in middle age.
However, in case of problems with the microflora of the skin, it is better to contact not only a dermatologist, but also a gastroenterologist and a nutritionist. After all, the skin reacts sharply to changes in the body, as well as to diseases of certain organs.